Fibroids: My Personal Experience of an Open Myomectomy & Recovery Tips

This post is for you if you are suffering from uterine fibroids and want to know what it’s like to have them removed by open myomectomy.
Fibroids are (usually) benign tumours of the womb. Mine was 17cm x 14cm x 10cm.
For my regular readers, this post might be a bit irrelevant as it doesn’t have anything to do with travel. So if that’s what you came here looking for, maybe have a browse through my Africa travel posts instead! 🙂
However, if you’re interested to hear about my personal experience with fibroids, fibroid surgery, and recovery, then read on…
DISCLAIMER: I am not a doctor and have no medical training, so I cannot offer any medical advice. This is just my personal experience. And even though I am a yoga teacher, I cannot offer advice on strengthening your core post-op, although I will tell you what I have done below. You would be best speaking to your own doctor or a physiotherapist who can give you an exercise programme that suits you and your individual circumstances.
I decided to write because as I haven’t seen many first-hand accounts of what it’s actually like to have a myomectomy, and if you’re going through this I hope it helps you to prepare for what’s ahead.
As many as 8/10 of you (women) reading this post will develop fibroids at some stage in your life. So it’s important to be aware of them – however, don’t be alarmed, in most women they cause no, or very little issues.
This is my personal story which I hope will help prepare you with what to expect pre and post-operation, as well as some tips for what to take in your hospital bag and the things I did to help me through it all.
This is by no means medical advice, but simply an account of my own experience. Please also feel free to share your experience in the comments below.
For the record, I’m 40-years-old and I have no children – but haven’t ruled children out.
You can read a bit of my fibroids history and everything I’ve learned from the experience here. But to give you a quick overview…
2023 UPDATE: Unfortunately, my fibroids came back and I had to have a hysterectomy in May 2023 (3 years after my myomectomy). You can read all about that here. This won’t be the case for everyone, but it was for me.

My Myomectomy Story
In late March 2020, I was admitted to hospital for the urgent removal of my fibroids. I’d discovered my fibroids in August 2018 after developing severe pains in my abdomen after travelling on bumpy roads in northern Namibia (I run tours in Africa for a living).
Back in the capital Windhoek, an ultrasound revealed the tumours. I’d always had quite severe PMT, bad cramps and heavy periods, which had been getting worse as I got older, but I just thought it was ‘normal’ and that was just the way my body worked.
When I returned home, a couple of months later, I was put on the hormone-blocking tablets called Esmya for the next year and a half. The aim was to shrink the fibroids and stop my heavy bleeding. The major downside of Esmya was that you need monthly blood tests to check your liver function as the drug can have some life-threatening side effects in rare cases.
If I had the choice, I would not take the drug again and as of March 2020, I believe the use of Esmya has been suspended.
The fibroids were annoying and twinged occasionally, but didn’t really stop me from doing anything. I travelled, went to the gym, surfed and I even climbed Kilimanjaro… but everything was harder, I felt heavy, anxious and as time went on, my clothes got tighter.
I felt very low sometimes, but I’m naturally quite a positive person so was able to pull myself up. It’s only now, after having them removed that I realise how badly they were affecting me.
An MRI scan in January 2020 showed that I had 2 big fibroids (which turned out to be 1 massive fibroid and 1 smaller one). I’d been on Esmya for over a year at this point and they were still ‘massive’ (my Gynaecologist’s words) so we decided it was time to check out my surgical options and I had an appointment with a surgeon booked for early March.

At the end of February 2021, whilst travelling in West Africa, the pains returned with a vengeance – again, after travelling on another bumpy road. Whilst this might not affect a lot of women with fibroids, mine were the size of a 20-week foetus, so having them rattle around inside was bound to hurt a bit.
When I got home, I also had Covid-19 and a bacterial infection picked up in West Africa which didn’t help and I actually think that the Covid may have worsened the fibroids (but I have no medical evidence to prove this).
I tried lots of natural cure remedies such as castor oil packs, celery juice, turmeric, hot water with black molasses and cider vinegar, you name it, but nothing really helped – I’d left it way too late for holistic remedies.
I spent hours in the bath each day as it was the only place where the pain subsided a little – our womb is connected to the water element (and our Sacral Chakra is in that area), so water is a very soothing place to be when the pains get bad. I also found that an ice pack helped, more so than a hot water bottle.
I recovered pretty quickly from my bout of Covid, but my stomach issues were getting worse (mixing a stomach bug with codeine isn’t a great combo) and the fibroids were agony.
I was in a lot of pain, but as my appointment was so close, I hung on, not wanting to be a further burden on the NHS at this terrible time. I was smashing the painkillers, but I was struggling to eat or sleep, and even walking was becoming difficult. I was in so much pain I couldn’t function normally. I stayed up all night watching TV, anything to distract myself.
But of course, with Covid on the rise, my consultation was cancelled.
But my pains just got worse and worse, to the point where I could barely function, so I asked my Gynae for an urgent appointment and when she saw me, she immediately sent me to the hospital.
I was shaking with the pain but after another ultrasound and some stronger painkillers they sent me home again, but after a few days, the painkillers weren’t working anymore – I cannot even begin to describe the way I felt, but I’ll never forget the worried look on my husband’s face as I writhed around our bedroom in pain.
The next morning I was back at the hospital.

Tests, Tests & More Tests
The pain in my womb was a dull but VERY intense pain but the pain on my right side (around my ovary) felt like someone was twisting a knife inside me. It was the worst pain I’ve experienced. Every time the doctor touched my stomach I burst into tears.
I could also feel the pressure on my bladder, bowels, and lower back. I was ready for it all to be over, I just wanted the pain to stop.
I know some of you will be feeling like this right now too. Please don’t give up hope. 3.5 months later, I now feel better than ever and the pain is a distant memory.
As soon as I arrived they put a cannula in the back of my left hand and took some blood for testing. They were concerned because of the level of pain I was in, so said they would need to keep me in for observation. Luckily, I’d brought a bag with me (see below for advice on what to bring) as I figured they might keep me in.
No visitors were allowed on the ward the whole time I was in the hospital due to Covid-19 so it was extremely lonely, but hopefully, when you go in for yours, lockdown will be over and visitors will be allowed.
Over the next 2 days, they took blood, urine, and stool samples. I had both internal and external ultrasounds as well as an internal exam.
I was given antibiotics for the stomach bug, and a mix of paracetamol (both in tablet and drip form) and Oramorph to manage the pain but I found it very difficult to sleep and would be up most of the night.
They sent me for a CT scan. When the results came back, it showed that the fibroids had had a growth spurt, outgrown their blood supply, and started to degenerate. They call this “the heart attack of the womb” due to the amount of pain it causes.
The fibroids were also pressing on my bowel and ureter and the doctors were worried about my kidneys being compromised. I also had a cyst on one ovary and the other ovary was obscured by the fibroid on all scans.
The surgeon told me I would almost certainly need a hysterectomy, due to the position of the fibroids on my cervix and that they may need to take out my ovaries too. They wouldn’t know until they did the operation.
He said that they would need to make an incision from my belly button down. I think most cuts are done along the bikini line now, but as my fibroids were quite large, they needed to go top to bottom.
I don’t have children and hadn’t ruled out the option of having them, so this news was devastating. I wasn’t ready to let go of my womb or go through menopause yet, so the thought of losing everything made me desperately sad. But my husband, family, and friends were super supportive and I mentally prepared myself.
But to be honest, I’d been in so much pain for so long by this point that I just wanted to be well again. So I told them to get in there and just do what they needed to do.
Myomectomy Operation Prep
My operation was scheduled for Tuesday morning. To my relief, the doctor allowed me to go home over the weekend before to get a bit of respite from the hospital stay.
I had to go back to the hospital on Sunday to give a blood sample, but it was nice to be able to be home if only for a couple of days, and not have a cannula in my hand.
Being alone, without any visitors made the days drag.
Plus, sleeping in a hospital isn’t always the easiest, because it’s noisy, you’re not in your own bed and they always wake you in the middle of the night to test your blood pressure, pulse, oxygen levels, and temperature.
On the Sunday evening, a friend’s sister sent me distance Reiki whilst I lay in the bath, with candles and soothing music playing. I was willing to try anything to make the pain go away. I was a bit skeptical, but to my surprise, it really worked.
Getting out of the bath, I felt a sense of calm and the pain had subsided considerably (even through the night) and I got about 6 hours of continuous sleep, something I hadn’t had in some time. I’ve since trained to become a Reiki practitioner myself – it was THAT powerful.
I returned to the hospital on Monday, with my operation scheduled for the following morning. That night, I messaged all of my female friends and asked them to send me their positive vibes, especially during my operation time, with a focus on healing my womb.
At midnight I went nil by mouth and tried to get some sleep.
Having My Myomectomy Operation
I was up early, nervous, and super thirsty, but unable to drink. It really helped just to swill my mouth with water, even if I couldn’t swallow.
In the morning I was visited by the surgeons and the lead anaesthetist. They asked me some questions, explained what was about to happen, and gave me the opportunity to ask some questions. I asked for a sedative, but they said it was too late, so I tried to stay calm with some deep breathing.
They explained that I would also have urology surgeons assisting because of the position of the fibroids on my ureter (the pipe that leads from your kidneys to your urethra) and they would be fitting me with a stent to protect my ureter, as well as a catheter during the operation – both are tubes that go up your wee pipe.
The catheter is fitted because it’s hard to walk for a couple of days after the op so you can’t go to the toilet, but from what I understand, it’s not that common to have a stent as well as a catheter.
The nurses gave me a gown and fitted me with a new cannula. They said I could wear my underwear, but as the surgeons would need to remove it anyway so I didn’t bother. I wore a dressing gown to cover my bum and a nurse walked me down to surgery. I was scared and my heart was racing, but I tried to focus on a positive outcome.
The nurse stayed with me whilst I got comfy on the bed and told me about her own hysterectomy. They gave me some inflatable massage socks to help lower the risk of deep vein thrombosis (DVT). The plan was to do a myomectomy if at all possible and just remove the fibroids, but I had to sign all of the relevant paperwork to allow them to take away the uterus and ovaries if necessary for my health.
That was a very strange thing to have to do, but I focused on being well again. That’s all you can do in that situation and I truly believe the mind is more powerful than we can imagine.
I was wheeled into the anaesthetist’s room where I met the full surgical team, all scrubbed up and ready to go. They were all serious, yet bright and cheery which put me at ease a little.
The last thing I remember was being told to shuffle up on my bed and the smell of anaesthetic – if you’ve had one before, you’ll know the smell I mean. They told me they were adding something to my cannula to relax me, but I was soon out for the count.

Myomectomy Hospital Recovery
Day 1
In what felt like seconds later, I was waking up in the recovery room with a nurse by my side.
When I came to properly, I couldn’t really feel anything, I was just glad to be awake and I looked around to see fellow patients, also coming out of their own surgeries.
I was wired up to a blood pouch and had an oxygen mask (as you can see above). They told me I’d lost a lot of blood during the operation and they’d had to give me a blood transfusion – this is very common with this type of surgery. They said they’d given me some of my own blood back, plus some donor blood.
I was drifting in and out a little bit when my wonderful surgeon came to see me. He told me that they had been able to perform the myomectomy after all and that both of my ovaries were ok. It was a miracle.
UPDATE: I had a follow-up scan which shows that I have one smaller fibroid left at the back, and they told me that the one they removed was 17cm x 14cm x 10cm.
Eventually, they wheeled me back down to my room.
I wasn’t in too much pain that day, as the anaesthetic was still in effect and my stomach was pretty numb. I had a very thick bandage/pad over the wound so I had no idea what state my stomach was in.
I was able to call my family and left a few very tired-sounding voice messages for people (listening back to them later was quite funny) but I was pretty wiped out and I wasn’t allowed to eat still, but to be honest, I wasn’t very hungry. But I was encouraged to drink lots of water to flush out my system.
The nurses gave me paracetamol and Oramorph throughout the rest of the day and I was prescribed iron tablets, as the blood loss had left me with anaemia. I also needed daily stomach injections (they didn’t hurt really and the needles are small – like diabetic stomach injections) to help prevent clotting and they would sporadically check me for signs of bleeding (both from stitches and vagina) – thankfully I didn’t bleed much really at all and my stitches stayed fully intact.
Most of the nurses just seemed surprised when they spotted the stent as some of them hadn’t seen one before.
It was weird to know that I had two tubes up there, but they weren’t that bad. I could only really feel them when I moved. It felt like mild cystitis. And it’s nice not having to worry about getting up to go to the loo.
One thing that they didn’t tell me, was how the anaesthetic affects your breathing.
Firstly, as anaesthetic stops your muscles from working, it also stops your urge to cough, so you get a bit of mucus build-up. So when you wake up, you end up needing to cough relatively frequently, but coughing after abdominal surgery is scary.
I held my stomach and did a kind of throat-clearing cough, trying to limit my movements and it was fine. It was a bit sore, but nothing you won’t be able to handle.
Your breathing will also be a bit funny for a day or two after your surgery. I kept feeling myself stop breathing for a moment when I was drifting off to sleep, a bit like sleep apnoea if you’ve ever experienced that. It’s nothing to worry about, but just be aware that it happens and it’s a bit freaky.
I also felt the need to tense my body a lot, almost like I was stretching, without actually stretching. This is kind of hard to describe, but it must have been another side effect of the anaesthetic.
Day 2
I’d slept pretty well overnight and I was allowed to eat today. I wasn’t very hungry, although I managed a little bit and I was super thirsty. I brought in some Ribena fruit cordial, which made it MUCH easier to get the fluids in.
I just lay there on my back for most of the day, watching TV, my massage socks inflating and deflating – they were getting on my nerves now. Again the nurses would come in to check on me every now and again, I had some more blood taken and they gave me another stomach injection.
I was prescribed two types of antibiotics (one was because I was showing signs of infection, the other was another round of the same antibiotics I was already taking due to the bug I’d picked up in Africa prior to my operation).
The surgeon came in to remove my stent. I was pretty scared about this, as they said he would just pull it out. I braced myself for pain, but it didn’t hurt – again it just felt like a little cystitis pain and it was only for a split second.
Once my stent was out, the nurses were keen for me to try and stand up. The thought of this terrified me. I was scared it was going to hurt and I was horribly weak.
Eventually, I plucked up the courage to put my legs over the edge of the bed and get to my feet, aided by one of the nurses. My stomach felt quite sore and it was really, really exhausting.
I felt like I might faint so got back into bed, wondering if I’d ever be able to move normally again (don’t worry – this is just a very temporary feeling).
That evening was probably the worst of all, as I was in a lot of pain. The nurses brought me all the painkillers they could, but I was in agony and my stomach was swollen. I thought that something must have gone very wrong. I cried and cried and begged for more painkillers but I’d had them all.
So the nurse called the doctor who examined me and confirmed that the pain was caused by… trapped wind. So she promptly prescribed me some laxatives and peppermint water.
Again, what they may not tell you (or at least I had no idea), is that you are pumped full of CO2 gas during stomach surgery (to keep you open I think) and what goes in, must come out. Albeit with a little help. Plus I hadn’t been to the toilet in days (codeine constipation).
I text my husband this: ‘Trying to pass wind feels worse than giving birth right now!’ Not that I’d know, and I’m sure it isn’t, but it was very painful.
So after a few big, long, strange trumps (you really don’t care when you’re in the hospital), the pain subsided to normal levels and I was able to sleep.
Day 3
The next morning, I was tired, but in a lot less pain than I had been and the next step was to get me walking and remove my catheter.
I managed to get out of bed and have a little walk around the room (holding my wee bag) but it wasn’t easy! I was so weak.
Plus, the catheter was really starting to annoy me but you can’t remove it until you can prove you can walk to the bathroom.
After doing a little lap of the ward, the nurse came in to remove the catheter, take my dressing off, and give me another anti-clotting injection in my stomach. I was able to take off the inflating socks too.
The catheter removal was much easier than I thought. They deflate the balloon inside you that holds the catheter in (you can’t feel that) and then the tube just slipped out. I didn’t even notice it coming out.
I was scared to remove the stomach dressing as I thought that would hurt too but it didn’t. However, I couldn’t bring myself to look at the wound just yet. Not yet anyway.
I then sat in my chair for a while. It took all my strength, but it felt good to be somewhere other than my bed. I was so, so tired due to the anaemia and dozed off to sleep numerous times.
A bit later, with the help of one of the nurses, I walked to the toilet. It was weird because I couldn’t tell when my bladder was full. It was the strangest sensation.
Going for a wee burned a little and it was pink, which they said was normal due to the catheter and stent likely irritating my bladder.
The second time I needed to pee, I went on my own, but didn’t quite make it and peed down my legs a bit. This scared me as I was worried my bladder was damaged forever, but of course, it wasn’t and that never happened again.
At this point, I still hadn’t managed to poop yet. The downside of painkillers like codeine and Oramorph, is that they bung you right up.
Day 4
On day 4, I managed to eat breakfast, get up, and shower. I felt pretty weak, but I did it. I didn’t really want to, but I think the motivating factor was that they said if I could shower and get about, they’d probably let me go home today – blood and urine tests aside.
Showering was weirdly scary. I was afraid of collapsing, afraid of the water touching me, and afraid of catching sight of my scar and fainting. It was weird to be scared of such normal, simple things, but Thankfully, I didn’t faint, I managed to look at my scar (and it looked a lot better than I expected) and the water was nice on my back but I didn’t let it run directly onto my stomach.
When I went for a wee, it still had a pinky tinge to it and the nurses said that it might be like that for a few days and it also burned a little, at the end of each wee. So it would feel normal, but as my bladder emptied, I would sting a bit at the end. Again, this is normal and went on for about ten days after the op…
Later that day, the doctor discharged me and I was allowed to go home.

Myomectomy Home Recovery
Week 1
This week I really took it easy – as my house was being renovated (dust = coughing, and as we know abdominal surgery and coughing do not mix well) I was staying with my brother, his wife and their kids, so I had lots of help.
You shouldn’t really do anything. No lifting (some say not even as much as a kettle), no hanging washing out, no stretching – lots of resting – both body and mind. I attribute my quick recovery to eliminating stress during my recovery too.
I know this isn’t always easy, but even doing some simple self-care practices such as meditating breathing or just staying off social media will help. And definitely take at least 2 weeks off work, 4-6 weeks if you work in a physical job and you also can’t drive for around 4 – 6 weeks after abdominal surgery.
I was taking a mix of ibruprofen, codeine and paracetamol (Tylenol for the American readers) for the pain relief.
After a couple of days (and some laxatives) I was able to go to the toilet again (again, it wasn’t painful like I was expecting), but with the iron tablets and anti-biotics, things weren’t quite back to normal yet and my stomach was upset. Iron tablets also turn your poo black – so don’t be shocked by that.
I remember one night, maybe around 6 days after my operation, I was super weak and completely spaced out, the anaemia had really kicked in. I could barely function. Some of you will already have experienced this when bleeding out, but I’d never had anaemia before, it knocked me for six.
But it passed and towards the end of the week, I was feeling much better. I made my own dinner one night, but it was really tiring to stand up for any length of time. It felt like I’d done a hundred sit-ups even though I was just pottering about the kitchen.
One thing that I did get, was a nappy rash on my butt. Almost like bed sores from all the lying down. I think it was a mix of wearing a hospital gown with no back for almost 3 days, lying on a pad (they put down these pads – like a puppy training pad – on your bed in case you bleed) plus my super sensitive skin.
My best friend is a nurse and she said it didn’t look good – so just watch out for that. It kind of snuck up on me. I just put Sudocrem on and after a few days, it went back to normal.
It’s important to not sit in one place for too long and keep a little bit active, even though you have to take it really easy.
My belly was still a bit swollen and I weighed myself for the first time, I was almost 2 stone lighter than I had been a couple of months ago – a combo of the fibroid removal and the lack of appetite in the weeks leading up to my operation and the few days after the op too. Even in that first week, I still ate very little.
I also managed to get more sleep than I’d had in weeks. For the first week I had to sleep on my back, and I would often wake up in a cold sweat – I’m not sure if that was the surgery, or the antibiotics I was taking.
But despite all of the above, I was feeling amazing. Very tired, a bit sore but nowhere near as sore as I was expecting – believe me, the pain prior to the operation was far worse than the pain after the operation (apart from the wind on night 2, and the laxatives/peppermint fixed that).
I got stronger each day, my stomach was still a bit swollen but much less swollen than before. And I was feeling so happy and grateful to be on the road to recovery.

Week 2 & Beyond
Each day I felt stronger. Once I stopped the antibiotics, my stomach started to feel a bit better, however, antibiotics can cause yeast infections – so be prepared for that and I was still on the iron tablets, so things weren’t totally normal in that department yet.
I began studying Reiki and Chakra Healing, the world started to become exciting again.
By the end of week 2, I’d stopped taking painkillers, only taking paracetamol if I needed it. I was able to move around more and walk a little further. My appetite started to come back and I even managed a glass of wine (just a small one).
My belly began to look a bit better, less swollen and stitches began to come out – I had some that dissolved and some that worked their way out. I began to rub Bio-Oil on my stomach to help with the scarring.
I’d mostly been wearing maxi dresses during recovery which really helped (try to avoid leggings and jeans or anything that’s tight) and I was spraying ‘My Expert Midwife – Spritz for Bits‘ onto my wound and taking Arnica tablets.
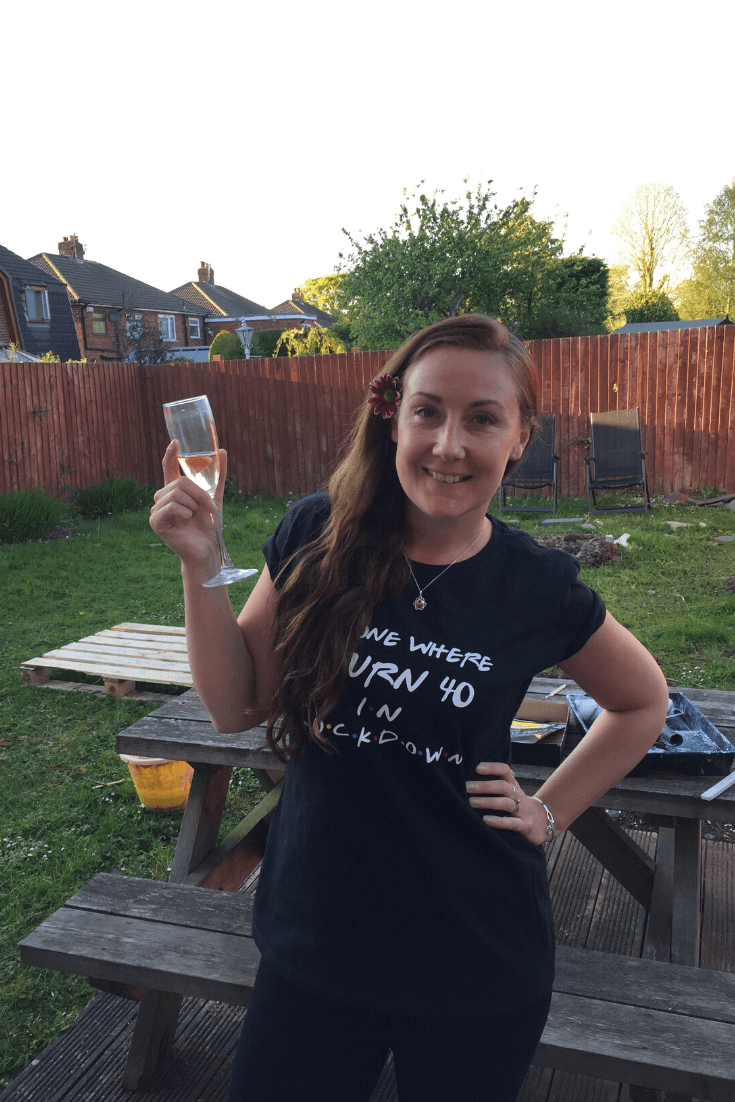
Each week I felt much better. In week 4 (my 40th birthday week), I attempted an online vinyasa flow yoga class. This did not go well and I felt sick after about 5 minutes and ended up sitting on the couch, watching the class whilst eating chocolate, and having a cup of tea. Thankfully, my video was off.
My scar was healing pretty well, although it started to spread a little.
At the beginning of week 5, I attempted another yoga class. This time I didn’t feel sick, but I may have overdone it and my stomach was killing me. I ended up going back on the codeine and having to rest for the night.

This didn’t last long though and by week 6, I was feeling a lot better. I was doing quite a bit of yoga (taking it easy on the belly) and the last bit of the external stitches came out. In fact, I was feeling great.
In week 7, I was feeling normal again and I began my yoga teacher training – albeit, I still had to (and still to this day) be cautious about the strain I put on my stomach.
Update: It’s now been 3.5 months since my operation and I am feeling better than ever. I’m a qualified yoga teacher and fitter and healthier than I’ve been in years. Although I would not suggest that you need to speak to your doctor before you begin any exercise, post-operation and don’t push yourself too hard.
I also went swimming with my 4-year-old nephew the other day and was wearing a bikini. He caught sight of my scar and shouted “Wow, Auntie Helen, your scar looks cool!” He approves. #badass #warriorwoman
Update 1: At the end of September 2020, approx. 6 months after my surgery, I developed a bad back (lots of stiffness stretching from my lower back, and to glutes and hips) which is likely due to me doing lots of yoga and my back over-compensating for my weakened stomach muscles. So the moral of this story is to a) be careful not to rush your recovery and b) work on strengthening your core, doing exercises that will not strain your delicate tummy muscles. After some physiotherapy and at-home exercises, back pains have gone, but they were pretty bad for about 3 weeks.
Update 2: It’s now November 2021. A year and a half after my surgery. All is good. I am so happy that I did the surgery. I’ve been exercising regularly and my bad back hasn’t returned. My stomach isn’t as flat as I’d like, but it’s relatively normal and I feel a million times better. I do not regret having a myomectomy one little bit.
I hope my story helps you prepare and also gives you hope for the future. Things may seem awful now, but there are ways to help get better, whether it’s holistically or via medical procedures.
Now my aim is to make sure they don’t grow back. I’m looking after myself, eating well, and taking time to rest. Life is good again and I intend to keep it that way!
Periods
Since I had my operation (3.5 months ago), I’ve had 3 periods. The first one came about 3 – 4 weeks after my operation.
They’ve all been much lighter and shorter than they were previously. The first one caused me to have quite strong, nauseating period pains (for a day, which required strong painkillers), but since then, they’ve not been bad at all. They are more regular and a lot less painful than they used to be.
Update: In November 2021, my periods are still pretty light, not that painful and much better than they have been for as long as I can remember.

Things to Take in Your Hospital Bag
- Soft nightie or pyjamas that won’t sit on your waistline (at least 2 in case you bleed or have night sweats like I did).
- Change of clothes (for when you leave). Again, make sure these are comfy, a stretchy cotton dress is great!
- Slippers.
- Warm socks – I had some thick winter Heat Holders ones.
- Dressing gown – I also used this as a blanket, both for warmth and something nice to cuddle.
- Big knickers – a few pairs of comfy ones, again that don’t sit on your waist.
- Sweater/hoody – it got cold in the hospital at times.
- Pillow – it was nice to have my own pillow as the hospital ones aren’t great.
- Books/computer/tablet – not all hospitals have tvs. Mine did but it was only free to watch in the mornings. Amazon Prime Video, Netflix and Disney Plus were my saviours.
- Phone.
- Charger.
- Headphones.
- Journal & pen.
- Toiletries – cleanser, moisturiser, toothpaste, toothbrush, shower stuff, shampoo etc.
- Lip balm – make sure you put in lip balm, as your lips will be dry and sore after the op. The one I use is O’keefe’s Lip Repair & Protect and it’s really good.
- Hairbrush – otherwise your hair can get a bit matted from lying on the pillow.
- A towel.
- Sanitary pads – you can’t use tampons for at least 6 weeks afterwards and you may have some bleeding.
- Hand sanitiser – I couldn’t always reach the stuff in my room as it was attached to the end of my bed so I wished I’d brought some.
- Vitamin C & Zinc tablets – check with the docs, but these are great immunity builders.
- Probiotics to keep your gut healthy! I was on antibiotics and they gave me a yeast infection.
- Turmeric tablets – great anti-inflammatories, but again, check with the doctor.
- My Expert Midwife Spritz for Bits – I started spraying this on the wound when I got home.
- Arnica tablets – to aid recovery.
- Eye mask & earplugs to help you sleep.
- Peppermint tea/oil – for the wind.
- Throat sweets – in case you get a sore throat after having the breathing tube in.
- Fruit cordial – I really liked having some Ribena with me as it helped me drink more water.
- Snacks/sweets/mints – in case you don’t love the food ( quite liked the food at the hospital).
- Crystals – if you are spiritually inclined these may help (Carnelian is a good one).
- Essential oils – lavender is a good all-rounder for calming/sleeping, orange for positivity, Albas Oil/eucalyptus for keeping your lungs clear.
My Tips for Myomectomy Recovery
- REST! The more rest you can get, the quicker you will recover. I mean this both physically and mentally.
- Take it super easy, especially in the first couple of weeks after the op. Don’t be lifting anything heavy or even anything light or doing any housework. Take it easy and let people look after you.
- But keep moving. Try and walk a little further each day, it will help you get back to normal quicker.
- If you live alone, make sure you have someone staying with you for at least the first 2 weeks.
- Make sure everything you need is close to hand so you don’t need to be bending down or reaching up.
- Be patient, it takes time to get better. Week 1 is the most difficult, but after that, it gets significantly easier.
- Keep an eye on your butt and try to avoid bed sores.
Tips for On-Going Life Changes (or at least what I’m doing to prevent my fibroids from returning)
- Listen to your body. going through an experience like this really opens up your eyes and your mind to what your body needs and wants. Listen to it. Notice if something triggers you, notice if a certain food doesn’t sit right for you – keep a food diary. The weeks and months since my operation have been the most ‘connected’ to myself that I’ve EVER felt.
- Get some sunshine if you can. They say that Vitamin D is really beneficial in the fight against fibroids and general well-being. If you live in a rainy place, as I do, I love this Vitamin D spray and take it every day.
- I also take the following supplements daily: Vitamin C, Zinc, Probiotics, Andrographis, and Turmeric tablets.
- Eat/drink healthily. This goes without saying, but there are lots of foods that are known/thought to help the fight against fibroids – leafy greens, celery juice, carrots, sweet potatoes, turmeric, grains, legumes etc.
- My friend recommends cutting out coffee/tea as they are acidic and you want to try and alkaline your body more.
- I recommend making tea from turmeric, ginger, lemon, honey, and black pepper. You can also add lemongrass. I love this drink.
- It is said that cleansing the liver is super important to regulate your hormones – this means avoiding high-fat, processed foods, red meat, dairy (although there are lots of contradictions around this), any foods with high-salt content, refined carbohydrates, sugar, caffeine, and alcohol. I’ve cut out milk completely and limited other dairy products with the aim to cut dairy out completely in the next few months (bye cheese – sobs).
- Avoid stress. I strongly believe that stress plays a major part in fibroid development. Stress causes hormone imbalance which messes with our bodies, especially our reproductive system. Watch the Netflix documentary ‘Heal’ and you’ll get an idea. Many of my yoga teachers also talk about this too.
- Yoga – I’ve found that yoga has really helped me recover. There are lots of yoga poses that can help fibroids and balance your Sacral chakra. Click here and here for two great classes. I also do my own practice with my own students which I’ll hopefully be able to share with you at some point. I also really love the classes by Tina Nance at The Yoga Barn, Bali – she teaches a lot about womb health and the Divine Feminine.
- In terms of exercises post-op, I have been doing exercises that strengthen my core and lower back, and that loosen up my hips (but just be careful to ensure that you are fully healed before you attempt any of these exercises), such as:
- Reclining butterfly
- Reclining windshield wiper legs
- Pigeon pose
- Planking
- Dead bug
- Bridge
- Breathe. Breathing exercises are amazing ways to calm your system and take time for yourself.
- Meditate – this is great for de-stressing and there are lots of guided meditations online for beginners, but if you want a super-powerful womb meditation, click here.
If you have any tips for other women suffering from this condition or want to share your own experience, please leave them in the comments below. Or if you have any questions, feel free to ask!







Helen,
Thank you for posting about your experience! I am scheduled for an open myomectomy in 3 days’ time – vertical as well. It is reassuring to hear you describe the exact same symptoms. After feeling gloomy about my whole situation – debilitating fibroids, being laid off work during a pandemic, surgeries and MRIs indefinitely suspended… I have to remind myself that those damn hormones are being manipulated by a puppet master in your private parts!
I previously had fibroids 9 years ago (I was 23 at the time) and had a laparoscopic myomectomy. Even then, doctors were not aware that if you morcellate the fibroid (cut it up into small pieces to remove it through a straw), it can spread throughout your womb and cause them to regrow. It was an overnight stay after the operation and I bounced back pretty quick… but now I’m in for round two.
The debilitating pain doctors say is due to cystic degeneration, caused by the fibroids outgrowing their blood supply, like yours. I’ve been aware of my 2 fibroids for 2 years now, was given Fibristal to shrink them, with monthly blood tests for liver function (shrunk 1cm and then grew back), and Tramadol pain killers, that I seem to run out of too frequently. It took a year for doctors to take my pain seriously. I was living off ibuprofen, hot water bottles, and screaming into a pillow. The MRI I just had in May showed the degeneration of the fibroids and the doctors finally realized that I was in fact, in pain. (eye roll).
The side effects of iron deficiency are endless. Not a great feeling, waking up with something in your body always bothering you. It’s fibroid roulette… will it be my uterus today, or will I just be dizzy with a headache, maybe it’ll be the black-poop constipation day! I can’t wait to go back to normal.
Despite so many women having fibroids, it’s still amazing how little we know about them, and the medical field hasn’t changed that much in 10 years. It was hard to describe to friends and co-workers that I needed a c-section for tumours… I look 6 months pregnant. The workplace support (ie medical leave/insurance) for fibroids is not quite there yet in Canada, but with stories like yours, we’ll get there soon.
I really appreciate the hospital check-list you included! My nurse said to only pack my medical card and a toiletry bag … how lucky are we to go through this amidst COVID!
Again, I appreciated your candidness in talking about your time in the hospital. I have not come across another blog or website with the details you have provided. You have reassured me and I feel more at ease for the next 3 days going into this surgery.
Safe travels! xoxo
Hi Cate,
Thank you so much for sharing your story with me too! Sounds like we are going through very similar things! We are very lucky with medical care in the UK, but I know women’s health can still be a struggle, even here. I think I was very lucky with the team I had in many ways.
Good luck with your surgery and keep a positive mindset, I really believe it helps.
Please let me know how you get on with your surgery – I will be thinking of you!
Helen xx
Hi Helen
Wouldyou be so kind to tell me which surgeon operated on you? I live in the UK, precisely in London…
If anyone has really good recommendations it would be very appreciated
Thank you for sharing your storyx
R
Hi Roberta,
Thanks for reading.
It was Mr Sharma at Ormskirk Hospital up in Lancashire. He also works at some of the private hospitals in the area, however it would be difficult to get home to London after the surgery (travelling that distance would be very uncomfortable), so I’d advise getting your surgery as close to home as you can. There are lots of great surgeons in London. 🙂
Helen x
Dear Helen: Thank you so much for your brave, detailed report. I was seriously considering surgery for my fibroid, that is estimated to be the size of a peach., and conducted a search to be better informed as to what to expect. I will be turning 67 this coming June, and my decision to go through with the operation was to improve the quality of the rest of my life. I am so grateful to have found your blog.
Although I am not in the pain you were in on a daily basis, but very uncomfortable, even to walk. I am tired often and my poor bladder is not happy with the constant pressure. I have been experiencing the severe lower back pain from time to time, which I did not associate to the fibroid until I read your blog. The daily bloating and peeing so frequently is extremely uncomfortable; if I need to go somewhere (grocery store, etc.), I have to think about where there is a bathroom I know I will need to use. During COVID, there were no bathrooms available.
When I was examined in January, 2021, including an in house ultrasound, my doctor discussed my options for removing the fibroid, and there was only one: surgery. Also, she said the removal of my fibroid would be outpatient surgery, in other words, I would be home by the end of the day. I feel that is not safe, and I should at least be monitored in a hospital overnight. I’m wondering if it is because I am on Medicare. I am going to talk with my doctor again to get some more realistic information about what to expect before, during, and after surgery.
Again, thank you for your informative blog. I know your article helping so many other women who did a google search on fibroids, like me, to learn more about the removal of fibroids and to make an informed decision.
Sincerely, Barbara
Hi Barbara, thanks for reading!
In terms of the surgery and how long to stay in hospital, it really depends on the type of surgery. I’m sure your doctor won’t suggest anything unsafe, but I’m not sure whether Medicare makes a difference or not. I had mine on the national health service in the UK and stayed in for 3 nights after surgery, but I had a full open myomectomy for a very large fibroid, but I think if you have smaller ones, they often do keyhole surgery so it’s less evasive/dangerous.
Definitely speak to your doctor and get all your options! I hope it goes well x
Hi Helen,
Your detailed analysis has helped me feel so much better already.
Thank you for taking the time to give an elaborate account of your experience with open myomectomy. I can relate to majority of the situations you’ve mentioned in your article.
Of importance is keeping a positive mindset, lots of rest for mind, body and spirit and not rushing your recovery journey.
Best wishes,
EmKay
Hi EmKay! That’s exactly right! You will get better, it just takes time… enjoy the rest time as we don’t usually get this much time to rest! 🙂 Turn the negative into the positive.
Wishing you a speedy recovery!
Helen x
Hi Cate,
I came across your reply through random search online and I’m also scheduled to do a open myomectomy soon in Canada. If you happen to see this, I’m curious to learn how your surgery and recovery turned out and what I could do to prep myself for the surgery in Canada (I’m in Toronto), as I’m feeling scared about the procedure as it’s the largest ever surgical procedure in my life so far.
(and Helen thank you so much for sharing your experience! I was so worried that having a open myomectomy may just ruin my normal being for the rest of my life but your post makes me feel better about my situation. My name is also Helen by the way).
Hi Helen,
No worries at all. What I described is exactly how it was by far the biggest surgical experience of my life too. It’s a big thing, a big operation, but… it’s also very common, so many women go through this but it’s just not talked about that much.
But, know this… I actually feel much better after my operation and it gave me a new lease of life! And, I hope it does the same for you. I feel mentally, spiritually and physically lighter! 🙂
Hi Helen #2!
I too was incredibly nervous before my surgery. Helen #1 was reassuring and by far the best insight I’ve seen online for fibroids. It wasn’t so much the surgery itself I was afraid of (I mean, all you have to do is go to sleep right?), but what to expect during recovery in and out of the hospital isn’t something you can find online and take comfort from (so thank you again Helen #1).
All I can say in regards to prep before your surgery, is clean you house, stock your fridge, make things accessible so you don’t have to reach or bend and lift, or leave your house for resupplying (toilet paper, pads, milk, egg, etc.) Buy some large underwear that goes above your belly-button. Pack light for the hospital. Whatever you were in, make it comfortable enough to wear out (I wore PJs and slippers). Drink lots of water the day before, because you won’t drink any the day of. And just breath in for 8 seconds and out for 8 seconds to stop the bounding in your chest 😉 The doctors and nurses know you’re nervous, so don’t be afraid to speak your mind. They offered me sedatives when I arrived, but the breathing really helps. My doctor held my hand as I went to sleep… it was soo cute.
I stayed in the hospital for 4 days after my abdominal myomectomy. To be honest, the whole hospital experience was pretty easy, I was just antsy and bored and wanted out. I recommend bringing a laptop or getting a room with a tv: the pain meds prevented me from focusing my eyes on a book to read, and a water bottle is a good idea since there’s no real access to it unless a nurse comes in. I just listened to music on my phone and brought a sleeping mask so I could sleep all day.
Everything went well in surgery. Woke up stoned and thirsty – you should ask them for a popsicle/ice in the recovery room! I had some pain initially when trying to sit and pee, but other than that I just felt stiff, and sore, and tired. The nurses try and get you walking as soon as your able, so I spent 4 days walking the halls, wheeling my IV and morphine drip everywhere … I was ready to leave on the second day! The only issue I had was a slight reaction to the Hydromorphone IV which gave me shallow breathing, low blood pressure and an itchy neck – oh but it felt good! Other than that, they slowly ween you off pain meds and make sure you poo and pee before you can leave. The doctors were really surprised how quickly I bounced out of bed to wander the halls and was willing to eat solid foods. Checked out of the hospital on the morning of the 4th day and went home – it felt great to be back in my own bed. I would recommend getting a family member to get your prescription meds for you, and let them take care of you for the first few days. I live alone, but my parents were nice enough to bring me food and check in on me!
Now, don’t freak out by this next bit! Apparently, it’s like a 5% chance of this happening to women who get the vertical cut; I went back to my OBGYN who was also my surgeon to get my staples removed from my incision. It didn’t hurt too much, felt almost like a scab burning slightly from being peeled too early when she pulled them all out. I got in the car and was just turning down the street when the burning got worse, suddenly I felt something come undone. I lifted my dress up and saw my entire incision had opened up. Yikes! Rather than going to the hospital and waiting in Emergency for hours to see a doctor, I went back to the clinic and the doctor rushed me right in and gave me 40 sutures. Wound dehiscence can happen for many reasons, a slight infection, an imperfection in the skin lining… It’s scary yes, and extended my healing process to 9 weeks instead of the normal 6, but everyone is different. Luckily the incision opened to the subcutaneous tissue (2nd layer). The scar was beautiful when the staples came out, now it’s quite large because the stitches just couldn’t make the skin taught enough and now it’s a bit ‘Harry Potter lightning bolt’. They gave me 7 days of antibiotics to ensure there was no infection because the incision was open and exposed while driving back to the clinic.
As I mentioned above, I pooped in the hospital, but after that I hadn’t for 7 days and then suddenly I had diarrhea for 12 days straight (up to 5 times a day) – it was exhausting, especially with the new lightning bolt sutures – I couldn’t drink enough water to maintain whatever this was that was going on, so I went back to the doctor. She checked the incision first, to which I had developed an allergy to the dissolvable sutures. This is also a thing that could happen to people with sensitive skin. She just cut the sutures out and my Harry-Potter-lightning-bolt-scar held up this time (shame really) … and she then sent me off for a stool test to figure out what was going on in an area that had nothing to do with Harry Potter.
48 hours later I received a phone call from the infectious disease centre, who told me I had Clostridioides difficile, more affectionately called in hospitals around the world as the nightmare bacteria: “C. Diff”. I was shocked and by this point, frustrated that of all the 5% of things that could happen, I seem to be checking a lot of boxes. After a decent pity party, my doctor explained that before surgery, they pump you full of antibiotics. Somewhere in those 4 days in hospital, I had contracted the bacteria and then… took more antibiotics after the wound opened and that stripped my gut of all good fighting bacteria. C. Diff can be deadly. So here I was, post-surgery, post second closer, unable to eat or drink, living on the toilet…
Fast forward to mid-October (2 ½ months post-surgery) first day back at work. It felt great to be around people (pandemic + surgery = hermit that has watched all of Netflix). Incision healed, C. Diff gone, but my periods are still heavy. I’ve undergone one iron infusion already. Doctors don’t recommend going on birth control for a while because you’re still susceptible to blood clots post-surgery, and they say if your period hasn’t ‘quieted down’ after the 2nd to 3rd month, then that’s the way it’s going to be (oh goodie). So, I’m still taking iron pills, and scheduled next week for my next IV iron infusion, and hopefully some good old fashion birth control to settle thee ol’ uterus down into a normal quiet life.
Yes, this is a horror story. But Helen #2, despite all of that, the surgery was still worth it. It’s good to hear a bad story, so you’re not surprised if the recovery throws you a few 5%ers. Despite all that, and the fact that there’s a pandemic going on, I’m doing all right. Getting better every day. I have good days and bad days, but I look back to where I was before my surgery, and I’ve come a long way. The only place to go is up from here. And hey, I’m only a 5% … chances are your surgery will be a breeze like Helen #1s!!
Please let me know how it goes!! xoxo
Oh wow Cate, thank you so much for sharing all this information and you are incredibly strong and positive! Your family and friends must be super proud of you, and I’m sure you can conquer any difficulty in life going forward after having experienced all these. I wish you all the bests going forward and I’m sure you will be doing better and better each day!
Helen thank you for your warm reply as well! I am really grateful to feel the support by reading your comment and Cate’s comment. I am grateful that you created this blog space where people can share their experience on this surgical procedure (and your blog and travel experiences are just really amazing).
I’ve been actually struggling to decide whether or not I should go ahead with the surgery. I have really mild if not zero symptoms although I do have a large fibroid (which was discovered by accident during a ultrasound). My doctor told me to get the surgery if I want to give birth in the future and he made it sound like the surgery is no big deal, but I really freaked out when reading more about the surgery online. I’m wondering why I should take the surgery, bear the pain and become not functional for many months, if I am fine right now. It almost feels like I’ll be “worse off” after the surgery. I think I’m also having all kinds of crazy mental thoughts like what I did to get myself into this situation, why this happened to me, etc. etc.
It helps to read you girls’ experiences and they sounded really tough but also promising as you both came out of the process stronger and healthier, and you were fine and you do not regret having the surgery. I hope to make my decision soon and I will keep you both posted on how it goes.
Thank you again and best wishes again!
Hey again Helen!
That’s tough, especially since your are aren’t experiencing any symptoms. This time around I had to really push the surgery route to my doctor. Her hope was I take Fibristal, a pill you take for 3 months, that is suppose to drink the fibroid. Once it shrunk, she said my options could open up, like laparoscopic myomectomy, which I have had before for fibroids, and that was an out patient procedure I did at sunnybrooke in Toronto. Sadly I just didn’t react to the meds like most people, but definitely talk to your doctor about options. I also took Lupron Depot injections last time, which made my fibroid weirdly mushy and shrink a bit to be removed laparoscopically. My doctor at Sunnybrooke in Toronto was Dr. Herb Wong.
Take time to consider your options. Whatever decision you
Make will be the right one for you!
Hi Cate, for some reason I couldn’t seem to reply to your last comment so I’m responding to this earlier one (Thank you again so much for your detailed answers and warm heart). My heart literally skipped a beat when I saw you mentioning Dr. Wong’s name as he’s actually my current doctor who’s going to do the surgery! I didn’t want to use Helen’s blog space as a chatting tool for myself, but I wish to ask you some questions about how your surgery last time with Dr. Wong went. So if you don’t mind continue corresponding with me you can reach me directly at [email protected]
(Yes, i created this gmail address so that I can ask questions about the fibroid situation…never thought I would do that before)
Also thank you Helen #1 for letting me leave all my selfish comments here and providing a space for me to learn about the fibroid surgery!
Hi Helen (and Cate) – Go for it! I love that you’ve found a space to ask questions and that I could be a part of that! I am happy for all the discussions you want to have! We can all learn from each other and everyone’s experience will be slightly different so it’s great to get different viewpoints! Good luck with the surgery, and please keep us all updated about how it goes. I’m so glad I had it, but I wasn’t getting to the point where I couldn’t function properly and it was really impacting my life. Now I feel SOOOOOOO much better and I’m sure you will too! xx
ps. I think maybe you couldn’t reply as you used a different email address and it may have gone into spam! x
Hi all,
So an update on my surgery (and Cate did find me via email, thank you Helen and Cate!)
I think my surgery went really well and the most difficult part was actually before surgery as I was so nervous that I could not sleep well. I remember I went to washroom for multiple times in the surgery waiting room as I was panicking and needed to do something to occupy myself!!
After the surgery, everything seemed to have gone better than I initially expected — I didn’t have the bad gas pain that lots of people seemed to have experienced, and my pain from incision was pretty manageable (at times I hardly felt any pain at all). I did get stomachache from the pain killers and I actually threw up the first day post op, but the first day post op was a blur so I didn’t remember suffering much or anything. I reduced my pain killer intakes after I got home (after a 48 hour hospital stay) and the stomachache went away after I stopped taking the pain killers.
Helen and Cate’s tips on what to bring to hospital were super helpful! I kinda overpacked as I didn’t a lot of the things I brought to the hospital (I didn’t use the pajamas, underwear or socks as I was just wearing the hospital gown). The stuff that I did find helpful: ear plugs, cell phone/ipad/charger, a sweater jacket, a water bottle for keeping water warm, tooth brush/tooth paste/face wash/hair band/face cream (I think I only brushed my teeth twice but it still helped to get refreshed).
Two things I didn’t bring but would be helpful: a container for my glasses (I had to stuff them into my winter boots in the surgery change room), and gums (the nurses said they could help with gas pain).
It’s now about 2 week and a half post surgery for me and I feel my energy level and comfort level are getting better and better. I’ve been exercising through walking outside daily (following advice I’ve taken from reading info on this blog) and the walking does really help with the recovery. I couldn’t walk very fast but at times I would feel really energetic to walk for a long time. The inside of my incision area hurts a bit from time to time for no apparent reasons, but overall everything is getting better. I’m happy with my recovery progress and I feel really blessed. I’m happy with my decision to remove the fibroids too as my stomach looks slimmer and healthier now (although I’ve been gaining some fat from eating too much and moving too little these days >_< ).
Thank you so much for the support and advice shared by everyone on this blog! I'll keep you posted on the progress of my recovery.
Hi Helen2!
So glad that your surgery went well! Been wondering how you were getting on!
Your experience sounds very similar to mine. The pain I felt before the surgery and nerves were worse than the aftermath, apart from the gas – ouch. But my incision itself wasn’t too bad, just hurt occasionally, but nothing I couldn’t handle. I think the fear of getting up after the op and the weakness I felt were worse than the actual pain.
I just wore my hospital gown after the surgery too, but wore my pyjamas to go home in (and to sleep in the week before the surgery). But I couldn’t be bothered to change into pj’s before that! 🙂
Keep us posted on your recovery. Send you lots of love and positive energy!
xx
Hi guys, I am 23 and freaking out cause I’ve never heard of Fibroid before. I am an International student, and cause of the lockdown I haven’t seen my parents. Coming to know about my fibroids was a shocker and I have my MRI test tomorrow. I am really nervous but thanks Helen your post has made me feel better. Though I have a question, do you reckon each case has to get a surgery done or can we delay the surgery for a while as it’ll be a bit cheaper in my home country?
Hi Manu,
Sorry to hear that you’ve discovered your fibroids whilst away from your family. That was the same for me and I know how scary it can be.
Don’t be nervous. The MRI is fine, if a little weird.
Not everyone needs surgery – some fibroids don’t cause many symptoms and most women have them at some point in their lives. You only really need surgery if they are becoming problematic.
Wait and see what the MRI results are and then make a decision with your doctor. Either way, there’s usually no rush unless the fibroids are causing problems, so waiting to you are home is probably an option! 🙂
I hope you get everything sorted soon!
xxx
Thank you so much for sharing. I had my fibroids removed a week ago. Unfortunately my experience was not as pleasant as yours. My removal was the same, cut from belly button down but when I awoke the next day I was able to rest most of the day but then by 7pm my doctor was ready to discharge me. At this point I hadn’t even tried walking or even standing and when I did the pain was incredible. The same pain you experienced. I told the nurse practitioner it was too soon and I was in pain. She told me the papers were signed and I needed to go home. The pain obviously got worse at home and I didn’t know what it was cause it wasn’t explained to me that it was gas till I went to the ER that night. I had no idea what was happening. Then my doctor readmitted me and took me off my pain meds and put me on a liquid diet. Then I slowly got better and stayed in the hospital another 2 days. I’m worried about the scar but I also know I could never have lived with them and it’s so comforting to read about someone having a similar experience. I couldn’t find any stories on it. Thank you for posting this!
So sorry to hear they discharged you so early – that’s ridiculous, no way should they have done that! The extra night in the hospital is 100% needed. Yeah the gas is the worst and the thing no-one seems to mention – it was the most painful thing I’ve ever experienced, orse than the fibroid pain. Luckily it only lasted a day for me and then I felt better after all the peppermint oil and laxatives.
Don’t worry about the scar, I love mine and my nephew thinks I’m cool! Hope you feel better soon – after another week you should be well on the mend!!! Hang on in there!! xxx
Hi Helen, was searching for pictures of post surgery scars and came across your blog. I had abdominal surgery 9 weeks ago and had a very similar incision and its reassuring to see how very similar our scars look at all the different stages. Its hard sometimes to know… is my scar as it should be, is it healing okay… so thanks for posting. I had surgery during covid too and you describe a lot of detail that I think will really help people. I had issues with bowel and wind pain after and I have to say it was awful and it sounds like we had a lot of the same drugs and recovery, although my issue wasn’t fibroid but a huge cyst that actually turned out to be a borderline tumour which has now gone along with margery the ovary! I’m still recovering, scar hurts sometimes and is itchy as hell, my full strength isn’t back but getting there. Love that you’ve given this account of your experience symptoms etc. Its going to really help others. You’re strong!
You’re so brave. Thanks for sharing this!
Thank you for reading. x
Hi All! I have read all the posts; I found this site now, at 11 weeks post open abdominal myomectomy.
I had 6 fibroids removed; I had no symptoms. My doctor insisted that not removing fibroids ( med to large) and waiting for symptoms or a bleeding ( or emergency surgery) was not a good idea. She is also of the thinking that the less fibroid-reducing drugs we take, the better and was completely against me taking them medium or long-term.
Fast forward to operation day: like all of you, I was very nervous. My doctor gave me two options for anesthesia: general or epidural. I went with the epidural and twilight so I would not be awake.
If you have a say, you might want to request stitches ( as opposed to staples) which are better in many ways. My incision was a bikini cut. My stitches were dissolvable but in the corners, I had 3-4 stitches that were removed on day 7. These corner stitches were extra protection in case the incision wanted to open.
I was in the hospital for 36 hrs. Given it was during covid, they did not want me there more than necessary. After the surgery, I had a catheter in my urethra so I would not have to go to the bathroom which was great; it was removed after 24 hrs, time at which a nurse said it was time to get up. The pain was incredible! I thought I was going to faint when I first got up. But the first one is the worst. The first 5 days were very painful. The catheter had also left a sensation which went away after about 2 weeks. Sitting on the toilet and getting up from the bed were the worst but after 5 days, I started feeling some relief. From days 6-14, I sort of felt the same and did not feel lots of improvement and was worried that I was not healing faster but after day 14, I again noticed significant improvements. Around week 4, I was feeling much better but my insides still hurt a lot when I coughed. The first time I allowed myself to sneeze was at week 6 because I was scared of the pain. Careful coughing was painful enough, let alone a sneeze!
Now, at 11 weeks, I feel I am at about 80-85%. It has been a slow process even though I have heeded all my dr’s recommendations: walking everyday starting day 3 and adding more walking time each week, making no efforts ( not even closing a window), not picking up or lifting anything, not laying in bed too long, eating well, not drinking alcohol for 30 days, drinking tons of water, using an icepack 3-4 times a day for 20 mins to reduce swelling, using Voltaren suppositories for the first 7 days to reduce inflammation, etc etc.
Starting at week 3, I started massaging my incision/ scar at my doctor’s instruction. This is to avoid adhesions and also to help flatten the scar. At the beginning I would just briefly rub it but with time, I started increasing the pressure and massaging “better” as I got more comfortable. I am also using a scar therapy gel called Strataderm; I definitely recommend you check it out.
After the surgery, I immediately noticed the overhang; I was looking at myself sideways every day and I was worried it would not go away but around week 6-7, I started seeing improvement here too. Now I am happy to report that the overhang has improved by about 80%.
I have had 3 periods. They are completely different now: the first day I will have very heavy bleeding ( changing pads every 1.5-2 hrs) and the rest of the days moderate/light.
I still have no sensation underneath my incision. Every person is different and the time for the numbness to go away will vary.
Sometimes I feel normal but most times there is a sensation from the surgery. It’s always reminding me it’s there. I am looking forward to feeling completely normal again.
Healing is not linear and not uniform. Some days will be better than others. The inside healing is also not uniform- I had specific internal spots that hurt more than others. I still have quick shooting pains and overall soreness. Today I lifted a semi-full suitcase thinking I am on week 11 and I felt discomfort and pulling. So hang in there! Every person is different. Even though my healing has take. A while, I am satisfied with my decision and I am convinced it was the right move for me.
Good luck to all!
Andrea
Thanks so much for sharing your story Andrea!
I too sometimes get some ‘pulling’ and did my back in because of my weakened stomach muscles. I need to remind myself to take it easy at times. I still have a bit of numbness too!
And I had that sensation you mention from the catheter too. I’d get like a burning feeling at the end of each wee! Went away eventually though!
I hope you get back to 100% soon. Thanks again for being so brave and sharing your story as I’m sure it will help and inspire others!
Helen x
Andrea, congrats on week 11! So glad to hear your surgery was a success!
It’s pretty crazy having to go through this with a pandemic eh?
I really enjoyed hearing your post-op recovery advice! That trick about massaging the incision is a great one. I’m about 7 months post-op and have been massaging it since week 6, it makes so much of a difference. My incision had this definitive sharp line feeling under the skin, from the subcutaneous and muscle cut and the scar tissue. It’s smooth now, and that ‘panus’ kangaroo pouch we all seem to acquire after the fibroid is gone, is shrinking daily. Definitely a water retention and post-surgery thing.
I also had deep sharp pains and it would get very bad after standing or walking longer than 30 minutes. About 3 months post op I still had it so I went to an Internist, who said, “yes it’s a major surgery, they do cut through muscle and nerves to access the uterus, those muscle and nerves will take the longest to heal so don’t beat yourself up if your healing process is taking longer than expected”. He gave me 2 weeks worth of gabapentin (for nerve pain) and it went away immediately and never came back. He said likely it was the nerves damaged and healing.
By week 11 I was still feeling week, but you’re almost there, and it sounds like you’re taking great care of yourself!
All the best,
Cate
hi,
your story was really emotional to me because I went thru the same procedure mine was also a life threating situation and it was very scary just the thought that if something happened to me what was going to happen to my girls who was going to take care of them I was in the hospital for 30 days with a covid pandemic it was so hard but thank God I survived took me 2 months for wound to heal, and still taking baby steps, It was really hard but always had faith.
keep strong
Diana
Thank you for sharing your story Diana. You’ve gone through such a big ordeal, and especially having your girls to look after too. What a fighter! Wishing you a speedy recovery. Take it day by, you will get there! Lots of love, Helen x
Hi Diana,
Thank you for sharing! Wow, thirty days in hopsital! You trooper! I am so glad to hear that you are much better now! Wishing you all the best! xx
Hi Helen. Just stumbled across this post as I am researching about open myomectomies. I am scheduled for an open myomectomy early next month, and I’d be lying if I said that I was not freaking out. I have one massive fibroid around 10.5 cm sitting on my uterus. I am only 23 years old and have never had surgery before, so I guess my biggest fear is going under general anesthesia. I am so nervous that I am going to lose so much blood/not wake up, or that they’re going to have to remove my uterus at such a young age. Your post, however, made me feel a bit more comfortable. I am glad that your operation went well and hope that mine will too! Thank you for sharing your story!
oops! I did not mean to leave my whole name if this can be deleted and I can re-write my post, I’d appreciate it!
I’ve taken it out before I published xx
Hey Katia,
Thank you for sharing. I know it’s scary – I had all the same fears as you. But at 23 you are young and your body is strong so I’m sure you will be absolutely fine. The surgeons are highly skilled and they do these operations all the time. I am sending positive vibes your way! Please let me know how you get on. xx
Hi Helen,
I’ve been following this post since last Nov., and it was sooo helpful, reassuring and supportive before and during my open myomectomy, and even now 6 weeks post my surgery I keep reading the new posted comments and every time it amazes me how common is this phenomenon and how little we know about it… so amazing how strong we can be as women- beings! so thanks so much to you and to the rest for sharing your stories :-).
And to Katia, I also had a massive fibroid (13cm)- and thank God the surgeons removed the fibroid and saved my uterus. The fears you’re describing are exactly the same as those i had (and on top of them was the fear that my tumor was malignant- which now I know was a ridiculous thought) – I wish I could ease and calm my fears back then and that’s why I decided to comment here – I just wanted to join all the wonderful and strong women here to reassure you and wish you a successful operation and recovery. The feeling I had after my op was as if my body had gone through a RE-SET mode – and through the pain, the weakness and sometimes the downs this feeling and knowing that I’m tumor-free were (and still are) powerful recovery-inducers – so whenever you have those frightening thoughts just focus on the fibroid-free stage- that soon all will be gone; the fibroid, the fears and the uncertainty :-).
Best wishes ❤
Hi Ala,
Thank you so much for sharing with us all!
I can totally relate to the ‘re-set’ that’s exactly how I felt too! Like a weight had been lifted, both physically and mentally.
Thank you for your wisdom and re-assuring words. I know there will be a few ladies who need to hear that right now.
xxx
Hi Katia,
I myself am a nurse. I have never had surgery before and shockingly I had same thoughts but then I asked myself…”how many patients do you know that never came out of surgery”? and the answer was 0. Anesthetic is very safe these days. You are sent into a very comfortable sleep with no recollection of it. Take it this way, the surgeons might ask you to count to 10. By the time you get to 8, you are out of it and before you know what’s happening , you are being woken up in recovery by nurses telling you it’s all over and you will have that confused look on your face like “what…what..how…that was quick”
That’s exactly how I felt too! It was like it was instantaneous!
HELLO Helen,
This blog was so helpful, thank you so much for sharing your experience. I have been searching for this for the longest time and just thought it is so sad that alot of women go through this but at the same time, alot of people are not aware of fibroids.
I too had my surgery in January 2021 through Private via referral from NHS and was the most scared I’d been my entire life. It was so bad that I did not tell any of my friends I was going for surgery until it was done and had been discharged.
I had nightmares as I had been reading a lot of risk during operation, that did not help at all.
I had 11 fibroids taken out all the size of a fist, the biggest being about 3 fist sizes but if you see me you’d never guessed that (I’m quiet small).
You have inspired me to tell my story and how I too have overcome this.
I have only over a week into my recovery and some side effect just don’t make sense to me but after readingyl your story, I get it now. I have this sharp pain that goes up and down my stomach to the chest, it hurts so much but it’s all just gas. I keep thinking there’s something wrong here and I’ve been getting it every single day.
I guess I am yet to discover more side effects and just know it’s nothing serious.
Thank you so much and I hope it all goes well for you.
Portia
Hi Portia,
Thanks so much for sharing your story with us. I hope your recovery is going well! After two weeks I started to feel much better. The first couple of weeks were definitely the hardest!
The gas is the worst, but I’d say to just keep taking peppermint tablets/oil and making sure to keep going to the toilet regularly, even if that means taking a fibre supplement for the first couple of weeks!
Please keep us updated on your recovery and I wish you good health. Helen xx
Hi Portia
Thanks for sharing. Were they able to keep your uterus? If you don’t mind could you share the name of your surgeon?
Thank you
R
Hello hun,
It’s been two months since my surgery and recovery has been soo good. I am able to move about alot more and getting to regular routine . I recently received a letter from the gynecologist that my uterus was not touch and is intact, so that’s great. I was referred by the NHS to private sector called BMI Hospital. They were fantastic!!! I hope this helps. Xoxox
My story is quite long so please pardon me
This blog helped me when I was researching in preparation of removing the fibroid. In November 2020, I had a scan which showed multiple fibroids and the biggest was 18cm. I also had some 16cms to 12cms and then little ones. I live in Australia and I am a woman of color(Fibroid is very common amongst us) so when every OBGYN I went to advised hysterectomy, my response was No. I sought different opinions. Yes I was aware I had super huge ones, my uterus was the size of 37 weeks pregnancy……literally full term. I knew the OBGYN’s were being careful plus trying to avoid risks but at the same time I knew hysterectomy was not an option for me. I was 33 yrs old. At the same time I know many women of color who have had huge fibroids removed…at some point I considered going back home to get the surgery done there because the doctors there were super experienced…I can only imagine how many they’d removed from black women in my country but then with Covid, I knew I couldn’t really travel so I continued searching for more OBGYN’s with experience of fibroid removal for women of color. I never discussed this with family cos I knew how fragile they were and I needed to be at a good head space to make decisions without anyone being overly emotional because of my options.
In November I reconnected with a friend with whom I had lost contact. Her husband was an OBGYN with over 25 years experience. We come from same country so when I heard he’d passed from cancer, it wrecked me. Normally I wouldn’t go to him for surgery because we were family friends(doctors cannot operate on family or friends here) but he was such a good man all round ….he had a good sense of humor and would have you pissing yourself laughing when you were around him….anyways I digress. I went and paid condolence visit to the wife and his adult children. After a few visits, one day the wife told me a story about her sister in-law in the UK(did I forget to mention her husband practiced in the UK as a consultant OBGYN for 16 years before relocating to Australia) who was 37 and had to have a hysterectomy for another health concern not related to fibroids. Then I blurted out(I guess I just had to talk to someone cos my friends and family did not know what I was going through) that my doctors were telling me same. She probed and I told her my story. She told me her husband before he died spoke highly of one OBGYN who also practiced in the UK for many years before moving to the Australia and she gave me his contact
Of course I called and made an appointment and within a week I was sitting in his office. He reviewed my scan and asked me “what do you want to do about this?”. I replied “I want to have kids”. He immediately replied “then that’s what we are going to do, we are going to get these fibroids out and preserve your womb/uterus”. Let me say here this man was the only OBGYN who I had met that asked me what I wanted without forcing his opinion on me. I liked him immediately.
He asked if I had concerns, I said I had concerns of bleeding during the surgery, he said he would minimize the bleed with a technique that I would not find in any text book. In summary, when he cuts me open, he would use a tube and tie the blood vessels connected to the uterus very tight so when he then proceeds to start cutting out the fibroids, the blood vessels that causes the bleed will not release blood cos they are tied tight to prevent any blood from escaping. Look at it this way, take the cap off a bottled water and turn it upside down. The water contents in that bottle will escape freely because the cap has been removed. But put the cap back on tight and turn the bottle upside down…the water will reach the cap but cannot escape because the cap is screwed on tight…That was what that the tube tied to my blood vessels was going to do. The surgeon told me that if he did not use this technique, I could loose up to 4 litres of blood in 1 minute
I booked for surgery and had it 25th of of January 2021 which was a Monday. On the Friday before the Monday I had to go into the private hospital for bloods in preparation. After bloods was collected, I went home and then returned on the Monday. I thought I would go into a ward before theatre but the anesthetist was concerned with the size of the fibroids…scan showed 7 large fibroids ranging from 18cm x1, 16cm x2, 15cm x2, x13cm x1 and 12cm x1 and then “little” ones….he was concerned of blood lust and booked a room for me at ICU post surgery which was why when I presented to the hospital reception, I was told I was to go to the day procedure unit and then after surgery ICU before regular ward once stable.
I changed and wore a gown. My surgeon came to the waiting cubicle and re-assured me that everything would go well. The anesthetist also came by…then it was time. I was wheeled into the theatre where I met the rest of the team which included nurses, surgical assistant and anesthetist assistant. The anesthetist gave me epidural before and then put a mask on me which was uncomfortable so I knocked it off. He smiled and said “okay I will inject the drug through your IV line then” and then I was out. This was around 2pm-ish. I woke up at around 7.30pm…and the first thing the recovery area nurse said to me was “everything went very well. You are okay now” and the tears I have kept inside of me for so long was literally streaming down my face. I was drowsy, tired, couldn’t talk due to the anesthetic but I was happy. I dosed off again. When I came to it the second time, I was able to talk…I had zero pain (my surgeon had given me nerve block before stitching me up) which kept me pain free for 3 days lol. I asked where I was the nurse told me I was in the recovery room. I asked if I would be going to ICU, she responded no that if I were, I would have woken up there…duhhh I knew that Oh did I forget to mention that I am a nurse manager….maybe that was why I kept insisting on different opinions before surgery lol.
The surgery had gone so well that I did not need to go to ICU. Then my surgeon came by and told me they had removed 26 fibroids and the biggest which the scan showed 18cm in November, was actually 25cm…wow. I was dizzy from that information. My fibroids filled out 2 big buckets in theatre. They drained the blood from the fibroids after they removed them and I lost some blood(700mls) so they gave me 2 units of blood while in theatre.
Anyways I was transferred to ward from recovery, slept all night and the following morning they gave me the anti blood clot injection(terrible decision for me) it thinned my blood and led to me bleeding. I didn’t even know I was bleeding until my physio came in and wanted to get me out of bed and we found out I was sitting on stained sheets. The surgeon stopped the injection and asked the nurses to administer Tranexamic medications IV to stop the bleed which it did. The bleed started to reduce to almost spotting. So they gave me another 2 units of blood. Before surgery, the doctor had ordered 4 units of blood. I had 2 in theatre and 2 on the ward.
By day 2 the physio had me working short distances with a walking frame to support myself and by day 3 I was pushing myself to walk without the frame to the annoyance of the physio who was concerned I could feel dizzy and fall…yep us health workers make terrible patients. I was ready for discharge by Day 4 but because I live alone and did not want anyone staying with me while I recuperate, they insisted I stayed a few more days until physio was confident. I also had not opened my bowels, so until I did a number 2, they were not going to discharge me. I also live in a 2 story house so my physio had me climbing stairs twice daily and by day 5 they were happy for me to be discharged which they signed off on for the next day which was day 6.
The gas issue I experienced was from day 4 actually. I asked the nurse for peppermint water-not tea and half an hour after taking the peppermint water, I was in the toilet farting seriously and doing a number 2. I had diarrhea till the following day and then it stopped.
When I got home, I was fine really. I stopped all pain meds by day 12 of surgery. The pain meds made me drowsy and I hate to lose control of my senses lol.
My sutures were the dissolvable ones so they just dissolved on their own. I met with my surgeon 3 weeks after surgery to know the histology of my fibroids…they were all benign. My surgeon advised I take 2 iron tablets daily to build up my haemoglobin but I hate taking those iron tablets. I waited another 2 weeks and then went to my regular clinic doctor who specializes in iron infusion and asked for one and within 4 days I was chilling at the clinic with iron infusion going up my veins…lol it is quicker and the iron is easily absorbed that way.
I resumed work on the 1st of March. My work is mostly desk job but I was bored to death at home and needed to start seeing normal people again.
I hope this story helps someone as Helen’s and others did me. Sorry it is long but I needed to tell the full story
I would also like to add that I had concerns of mucus(I suffer from post nasal drip. I wake up in the morning with my throat full of mucus that I have to cough up) build up when I woke up due to my body not being able to cough while under anesthetic but when I woke up, my airway was very clear. Apparently the anesthetist suctioned all the mucus before he brought me out of anesthetic. I guess that was why my throat/airways was clear with no issues
Hi Joy, thank you so much for sharing your story with us! Wow, those were big fibroids!
I am glad you got them removed and your surgery went well!! I hope you are feeling much better now – it makes you feel so much lighter doesn’t it! 🙂
Take care of yourself! x
Hello Helen!
I hope you are well.
I just want to say thank you for sharing your story as I too a 40yr old fit young lady has been struck down with a large, not as mahoosive as yours! Fibroid.
Mine in october 2020 was 7x7x6cm so a tennis ball and I was caught out in june whilst teaching a spin class (outside) with a big bleed out. So embarrassing.
I begged drs for help but they put it down to stress of leaving a 16yr marriage and lockdown.
Eventually a dr stated that this wasnt just periods and sent me for an ultrasound…..tgis was october. Once I was told what was wrong with me I had to do a lifeguard shift with 101 questions running thru my mind…..why me? What have I done wrong?
Even after reading up about fibroids I had more questions…..I’m not over weight…..well not fat wise….its muscle.
I’ve come to terms now with it and this week I’ve now had my pre op appointment and blood test this week, so hopefully I will have an open myomectomy soon.
Reading your blog has given me hope and a positive energy to go into this operation.
Reading so many articles about ladies in the US makes no impact on me…however you have.
Thank you so much.
Positive vibes, peace and love
Frankie
Hey Frankie, thank you for sharing your story!
I felt the same, what have I done to bring this on myself. I think I said to the doctor, is it because I drink alcohol and eat cheese and he told me off for blaming myself. No-one really knows why we get fibroids and I think it’s a combo or genetic disposition, stress, hormones and maybe some environmental factors.
A friend of mine recently said that I should cut out everything that isn’t plant-based but then I read the vitamin A in milk and eggs helps fibroids. It’s so confusing! I am sorry this happened to you and I hope you get sorted soon! The myomectomy was fine and I’m glad I had it. There are ways people can suggest to shrink them naturally, but it can take a long time. Once you’ve had the operation take it easy and especially try and limit any stress in your life. xx
I came across this post by simple search in google for open myomectomy and all these stories inspired me so much. You are all so brave and strong and especially staying positive throughout the operation and recovery!
I too have very large fibroid (I think the largest is 9.8cm), or shall I say, multiple fibroids various sizes(don’t know exactly how many) and I have been advised on the open surgery to remove fibroids. I am very scared and don’t know what to expect, it came as a shock when I heard word “operation” first time. Now I am getting used to this thought and reading through your posts it gives me hope that it will all go well. 🙂
I had my initial consultation with the surgeon and he suggested open myomectomy is the best solution.
I also read a lot about different options, such as artery embolization and some laser therapies, however each story is unique and some not suitable for those. I really wanted to do a laparoscopic myomectomy instead of open, however I have been advised that it won’t be possible for me as my uterus so enlarged that it’s going into my stomach. They want to give me Prostap to try and reduce the size before operation and if this will respond well, they might review laparoscopy solution. If not I will have to go for open vertical cut. This scares me even more and a lot of thought in my mind for my life after and having a visible scar for the rest of my life (I am only 31yrs).
But I am staying positive and don’t lose hope for the best solution and the best outcome.
Thank you so much for your posts, it’s really gave me that second breath of home.
I wish you all a speedy recovery with no complications and returning to the normal life. Strength and positive vibes from me to all you beautiful and super strong woman, mentally and physically!
Take care of yourself xx
Hi Alina,
Thank you for sharing your story and the well wishes to everyone. Please don’t worry about the operation. I am sure you are in the best hands! It was the best thing I did and made me feel so much better. Immediately my mind felt lighter and happier. And don’t worry about the scar. I was worried too, but I actually love my scar now. It is fading a lot. I can still see it, but it’s a lot less than last year.
Please let us know how you get on! Sending healing vibes! Helen x
Hi Helen
I just came across this post and found it so helpful-specially because it’s so personal. I had my myomectomy on Monday night (it’s Friday now).
It’s also weird because I’m in travel in South Africa too, I run a specialist tour company in Joburg Inner city-anyway not relevant here.
I’m 4 days in, and my operation went pretty similar to yours, was strangely comforting to read your experiences. I also waited for mine due to Covid. It went well except I had a bad reaction to the anaesthetic and then the pain pills.
But I must say I’m really struggling with a bloated tummy tonight (a mix of sort of numb vs painful bloat) and terrible reflux. Luckily my tummy has started to work. Still feeling really awful and can’t get comfy lying down or on my side.
I also struggle to not do everything and need to learn how to let go and relax.
Anyway thanks for the comforting words!
Jo
Hi Jo,
Thanks for sharing your story! Aw, you are right in the thick of it hey!! The bloating and swelling will go down in the next few days and then it’s just a case of resting so your middle can repair itself (which it will, even if it doesn’t feel like that now). Lying on your side will be difficult for the first few weeks, so try to sleep on your back with your top half slightly lifted, with pillows propped all around. I would lie on my back, but the mountain of pillows on either side of my head allowed my head to go to the side (my preferred sleep position) but for the rest of me to be on my back. So basically, I was just twisting my body from the chest up.
And relax!!!! Don’t lift anything heavy!! I hope you feel better soon (you will, I promise).
Ps. I’ve heard about your tours. I will get back in touch when I’m back in Jozi. x
Hi Helen, I’m so glad I found your blog. I’m 42 and have just received a letter for an open myomectomy on 26th march 2021 , 4 days after my 43rd birthday!!
I’m petrified as I have quite bad memories of being in hospital when I had my c section 25 years ago. I had postnatal depression and I was a young mum with no support. I’m scared of the pain, the scar and if something goes wrong. Basically im scared of everything lol.
My fibroid is 20 cm all round and my uterus is the size of a 32 week pregnancy. I knew something was wrong in 2019 as I’d never had a large tummy but I thought I’d just put on weight. By Jan 2020 I decided to get it checked out because my stomach felt hard.
I had an ultrasound confirming a fibroid and in May 2020, I had an MRI scan. I had a feeling of pressure and back ache most days and everyone thought I was pregnant.
I was prescribed prostap injections to shrink the fibroid from September 2020. It did shrink somewhat and my period stopped , which was great as I was haemorrhaging each month.
Like you , I’ve been told it’s too large for a bikini incision so I have to have a vertical cut. I’m so scared I feel physically sick and anxious. I feel angry with myself for not taking care of myself better and possibly preventing it from growing to this size. After the surgery , I’ve a made a promise to eat better and get back to the gym ASAP.
I feel that I might be depressed afterwards because I live alone and lockdown has been hard for me. Its going to worse when I’m in pain , alone and feeling vulnerable.
I’m hoping towards the end of my recovery I can book a holiday. Africa is definitely on my list of places to visit. I can’t wait to get some sunshine and feel happy again . This is what keeps me going.
The tips you’ve shared are so helpful, so thankyou so much. I feel a bit better having read your story. Would you recommend an abdominal binder to help with walking and when I need to cough?? How bad is the pain??
Hi Michelle,
Please don’t be scared! The medical staff know exactly what they are doing. The pain wasn’t as bad as I expected and it was only bad for a day from the gas. The rest was more sore than painful. Mentally, it’s different from the way you might feel in terms of the hormones running around after pregnancy. For me personally, I felt a huge sense of relief after the surgery. I felt lighter and my mental health was better than it had been in years.
But I would suggest having someone help you for the first week at least, if you can as it will be hard to do stuff around the house. But f not, don’t worry – just make everything easy to reach so that you don’t have to strain yourself. Do your shopping beforehand too so that you don’t have to go out at first or do any lifting. Have your friends/family on standby to video chat if you need!!
As Frankie says, don’t beat yourself up about the cause of the fibroids. Some of the ‘healthiest’ women I know – vegans, personal trainers, and yoga instructors have fibroids – it’s nothing you did.
I didn’t have a binder, so hard to say but the pain wasn’t that bad. When I coughed it was more uncomfortable than painful and I think my fear was worse than it actually felt. After a week I was walking around pretty normally (if a bit slow) but my stomach ached after a few minutes of standing – but again, not painful, more just achy.
Please let us know how you get on! Sending lots of positive vibes your way!! x
Thank you. I have taken on board some of your tips and im trying to think positive.
I’ll update you in a couple of months and I may book a trip to Africa to treat myself !!
Yay! You will definitely deserve a trip to Africa after this! 🙂 x
Hi Helen, I’m two weeks post op and I’m doing OK! I had one fibroid removed, the surgeon said it was 25 cm and weighed 4lb! I had staples to close a large vertical incision from my pubic area to just above my belly button.
The incision size was a shock and it’s hard to look at right now, but with time I hope the wound heals well and there is minimal scarring.
The nursing staff were all lovely which helped put me at ease during my three day hospital stay.
I still have pain but I’m taking pain killers every few hours and recovering slowly.
Thank-you for sharing your experience it has really helped a lot of women prepare for this invasive procedure.
Hi Michelle,
Thanks for letting us know how you got on! I know that feeling of not being able to look at the incision, but it will get better and heal.
And you are very welcome. I wanted to share it as I hadn’t seen many first-hand accounts online.
Stays strong and I am wishing you a speedy recovery!
xxx
Hi Michelle
As a fellow fibroid sufferer and I’m sure Helen will back me here…..dont punish yourself for the fibroid.
I’m a 41yr old fitness instructor and lifeguard…never been pregnant…fibroids are a mystery to the medical world as to why we women get them and why they effect some of us and not at all for others.
I too went thru wondering why I got 1 too and as Helen told me…its not my fault. That’s not to stop you from wanting to go to the gym and eating healthy it’s to let you know not to be too hard on yourself my dear
I’m glad you have a date…..I’m awaiting mine….stay safe and positive.
Big love and positive vibes xx
Thanks .
I have really found this blog the most helpful and will keep you all posted. I know I shouldn’t blame myself but I do want to make an effort to sort out mu diet and hormones after the op.
Hi Michelle, best wishes for the op!
Re the pain post myomectomy it’s not that strong that a regular painkiller can’t treat – and if not you can ask for a prescription for a stronger painkiller from you gyn. – so don’t worry about it :-).
As to the ‘what I’ve done wrong’ part, 9w post my myomectomy another (smaller) fibroid was discovered in my uterus that was missed out in the scans before op (the massive fibroid displaced my womb in a way that made it hard to clearly scan the interior of the womb) and I keep thinking what I’ve done wrong, what if I treated the larger fibroid on time when I first felt it, what if I went for alternative procedure, what if I went to a different clinic…. yesterday I had a consultation with (a new) Gyn. and he said that I’m being hard on myself, that fibroids are so common and I can’t know when it all started so I shouldn’t blame myself.
I know it could be tough and frustrating sometimes – but it’s what it’s and we need to adapt to the new challenge and do our best to cope with it- both physically and mentally as this shall eventually pass :-). I also know being alone during the recovery is not easy specially with the pandemic – but it’s not impossible – i mean we’re strong- aren’t we (and the scar made me feel stronger, made me think that you have to be so strong to have a scar ;-). Helen’s nephew said her scar is cool – and yes I do relate to this too 😉 )?!
Best wishes â¤
Hi Ala,
Thanks for your encouraging words!
I too have a fibroid left over that I think they missed that couldn’t be seen on the original scans. When I had my op, I thought they were all gone, but when I went for a scan a few months later I still had one smaller one.
Just one of those things I guess!! I’m keeping an eye on how I feel and how my body behaves now!
Thanks for the words of encouragement. I will try and stay positive. X
Hopefully your small fibroid stays small and dosent cause you any more issues .
Hi. Thanks for all the helpful information. I’m Day 2 post/op from an abdominal myometctmy. I’m a 41 year old with no children and did not want anything major done that would not allow me to have kids in the future (should I decide later on). I had no period issues but the fibroid was large enough (close to 9 cm) that it was pressing up against my bladder causing frequent urination. In addition, I have a small frame so the mass would make me feel severely bloated (enough that I had to buy Spanx for some work dresses). My GYN suggested the open surgery as it would remove the large dominant fibroid and a smaller one that was spotted on the ultrasound. I asked what other options were available and she said I could monitor it but it wouldn’t likely shrink and now that I showed symptoms there wasn’t much more to do but have it removed.
Fast forward to early March 2021, lots of COVID protocols in place because I live in NYU. I had the surgery on Wednesday and spent the night in the hospital. I went under general anesthesia and had no block. Woke up in recovery and felt ok but really tired. My blood pressure dropped a bit but we were able to stabilize it with some extra drugs and more hydration. They said I needed more fluids. I was transferred to a private room and spent the day getting IVs and more pain meds (a cocktail of Tylenol, prescription strength Motrin, and Oxi). I didn’t attempt to get out of bed until after dinner and it was super painful. I consider myself active and even sitting on the edge of the bed was difficult. Finally made it up and they wanted me to pee (I had to get a catheter because I wasn’t able to pee post recovery and my bladder was full). I was able to pee fine and it was a relief. I walked around the hospital floor holding a nurse’s hand. It was pretty painful. A few hours later I had pretty severe gas pains. Not a joke. I called the nurse and asked for some gas meds. I wasn’t able to pass any gas for a few hours. Gas pains are painful because they were so sharp. I went to the restroom again and walked a bit around the floor again (this time without holding on). Progress! A few hours later I was able to walk again and the pain was a bit better. Slow and steady wins the race. It was very difficult for me to sleep in the hospital because I was super uncomfortable and the nurses kept coming into the room for monitoring.
My surgeon came by to visit a few times to tell me that everything went well and that I could be released in the morning. I was finally able to see the wound and it was pretty black and blue and swollen. The actual incision is pretty small (about 3-4 cm).
I was discharged and they gave me some Oxi for the travel home. I met my parents in the lobby of the hospital and we got a cab. Unfortunately the cab driver did not seem to listen to my instructions of “please drive slowly†and “avoid pot holesâ€. I tried to support myself as best as I could but it was painful to go over bumps.
Once I got home, I had some lunch and I took my next round of meds. Unfortunately the Oxi made me sick this time around (I later learned I was on an anti nauseous drip at the hospital). So I talked to my doctor and she said to skip the Oxi for now and just rotate Tylenol and the Ibuprofen. So that’s what I’ve been doing. Walking and getting out of bed still is painful but not as terrible as it was in the hospital.
I recommend asking for maternity underwear to wear home. It’s gauze material, high waisted and briefs. I have been using them and I find them very comfortable. I have started to ice mr wound around slightly.
I’m still pretty sore and tired. I know time will tell. It’s tough to just exist but definitely something I need to do. Happy that I finally removed this large fibroid because it was becoming so annoying and impacting my daily life.
Thank you for sharing your story Dana! Wishing you a speedy recovery! x
Hi Dana!
I’ll have fibroid surgery next Monday. I’m scared as I never had a surgery before. My surgeon said he will need to do an open myomectomy as he will try to preserve my uterus. I’m 38 and would still like to leave the chances open. Apparently, I only have one with 9/10 cm intramural and submucosal, located in the posterior part. I think I’ll opt for general anesthesia due to my anxious personality. It’s better not to be aware of what’s happening in the operating room. Also, my surgeon said it would last about 2hours. Send me positive vibes, please. Everything will be okay!
Hi Helen
Your blog on this subject is AMAZING! Thank you so much for taking the time to put it out there, despite it being nothing to do with your work and simply as a helping hand to others in a similar situation. That’s such a kind and generous thing for you to do and it’s been a really positive, insightful and useful blog to read. I’m having open myomectomy on the 6th April for two large fibroids and currently getting together all the things I need to get me smoothly through the op and recovery. Again, I can’t thank you enough for your thoughts and for detailing your experience. It will be my go-to resource and one I feel I can trust. I’m so glad I came across it!
I live on my own, but to start my recovery, I will be with my mother for 10 days after the op. Then I’ll go home. I live in rural Somerset, so it will be super chilled and calm…and although I’ll not be able to drive, I can call on friends to bring me groceries and that kind of thing. The writing of your experience in chronological time is really helpful to bear in mind as I make my plans, as are the lists of what to bring to the hospital and also thoughts to homeopathic remedies, peppermint oil (who knew…and do you take it in water?) breathing meditations and thoughts to iron replacement. I find the iron tablets really bung me up and just so you know, unsulphered apricots are packed full of the stuff and in easily absorbable form.
Also, I’m really intrigued as to your reiki training…did you do it online? As you were healing? If so, what a brilliant use of a less active time! I might have to look into it myself. Any pointers on this would be hugely appreciated.
And to all the other wonderful and brave women here who have already had their ops…sending love and light for speedy healing, on all levels. Same too, to others preparing to go in.
x
Hi Jane,
So glad the post has helped you!
You sound like you are all prepared and the first few days are the most difficult so if you have your mum around, you’ll be grand and then if friends can help you after that, that’s great! Rural Somerset sounds like a wonderful place to recuperate!
Yes, the peppermint oil you can take in water. They actually gave me this at the hospital. The iron tablets may only be needed if you have a blood transfusion like I did – so you may get away with it!
And yes, I did my reiki training online through Teachable, although I’d love to do an in-person course too.
Good luck with everything and please let me know how it goes!! Wishing you a speedy recovery! x
Hi Helen
What if someone has no help? Wpuld they be able to go through the recovery anyway?
You should be fine as long as you prepare before ie. moving things into a position where they’re easy to reach, getting shopping in before you go into hospital etc.
Thank you for replying Helen. I am very grateful for your response and the brilliant idea of creating this blog
How long for where you in pain after surgery? Do I need a sofa as well as a bed?
Thank you
No worries!
I stopped feeling major pain after a few days. When I left hospital it was sore but not what I’d call painful.
It was sore for a couple of weeks, but then I started to feel pretty normal – but still took it easy for about 6 weeks. I found that I
You don’t need a sofa but if you have just a bed, I’d make sure you have good cushions/pillows as it’s sometimes more comfortable to sit propped up.
Hi Helen! It was great to read your story. I had my fibroid removed too just 5 days back through open myomectomy. It was 21×17 cm. I developed fever and excessive shivers right after the surgery while on blood transfusion. I couldn’t eat for more than 24 hours cause I was in pretty bad shape. Finally when I started having liquids, I vomited all of it and had to be on drips and get injected several times. Anyway, I felt better the next day and could finally have liquids and soft foods. I got discharged two days after the surgery and am recovering from home. I’ve been walking at slow pace and taking good rest. I do feel a little pain before/after urine but I hope that is normal.
Thank you for sharing your story. Doesn’t feel alone going through this journey. Kudos to all women out there who underwent the surgery bravely; and to all women who are to take the surgery – be brave, everything will go just fine.. you’ll be glad you did it.
XOXO
Hi Gracy, thanks for sharing your story! So sorry to hear you had a difficult time after the surgery! But glad to hear that you are on the mend now!
The pain after you go to the toilet is normal – it’s usually just where the catheter has scraped your bladder but it should heal after a week or two. If the pain persists, speak to your doctor.
Sending you lots f healing vibes xxx
Hi Helen,
thank you for your post and to all the ladies sharing their experience. I just had fibroids removed about almost 2 weeks ago. indeed, for me, the first week was really painful and I felt everything you described. Now, it has been almost 2 weeks. I feel way better than the beginning. it still hurt a bit but nothing that i cannot handle
my belly is still a little bit swollen and the area around the incision some part are still a bit swollen and hard.doctor said it will go down. I have to admit it is freaking me out. Also, I noticed the skin on my belly is tender, like sensitive, but only if I touch.
I am happy to read you ladies as I was looking everywhere where the subject will be more specific, especially all that happens once you are home, what to expect without panicking.
really thank you ladies.
Hi there. I’ve read your blog and I’m 4 weeks post op today and in the middle of the worst period of my life – I feel like crying. What I wanted to know is if you felt slight pain/pressure when sitting after your myomectomy. Up to today, I sit gingerly because I feel slight pressure when sitting and tension up to my incision. Also, how long did your pain from surgery last?
I’m two weeks post op today and yes its uncomfortable to sit on my sofas. I am tempted to buy a recliner chair as I believe this will help me feel more comfortable. You could try purchasing one or even a secondhand one. In the meantime I’m propping myself up with lots of pillows. I can’t lay flat at night either . I sleep propped up on my back. If you need to cry then go ahead, don’t hold it in. The procedure can be stressful and traumatic on the mind and body. I’m still in pain; lots of sharp shooting pain and stomach cramps. We all have bad days but it will get better . Xxx
I spent a lot of time in the corner of my brother’s corner couch with my feet up or in the garden on a sun lounger (I was recovering this time last year when we had that great weather) as it was more comfortable than chairs!
Get better soon lovely! xxxx
I had my surgery on March 31st 2021. I’m on day 11th of recovery from my open myomectomy. It’s hard. I’m a single mom with 2 children ages 11 and 9. They help me, but kids are kids. I live in a foreign country without family, friends living far away. So from day one I’ve been doing for myself.
I have post op appt on April 14th 2021. Hopefully it goes great. I’m still feeling very uncomfortable and close to lower abs in the middle is swollen. I can press on the left and a little of the far right but not middle. I pray everything is ok.
Thanks for sharing. Hope all is well now.
Hi Bianca,
Thank you for sharing! I’m sure everything is ok – 2 weeks is still very early days and you have 2 kids to look after too. Just try and take it easy and get them doing any of the bending and lifting! 🙂
Good luck with your post-op!! Sending lots of love and healing vibes your way!
xxx
I read your stories and I am as they say “gutted”.
My wife aged 25 at the time had fibroids. but she got
rid of them through dieting.
When we went to see the surgeon at the hospital
he confirmed the fibroids had gone from a scan and
so there was no need for an operation.
My wife tried to explain what she had been doing
with her diet but the surgeon didn’t want to know.
She went on to have a healthy baby boy three years
later. No sign of fibroids.
The way I see it the cause is likely estrogen dominance.
so what is the test for estrogen dominance and
what can be done to balance the hormones.?
where is the estrogen coming from? What are the
likely possibilities.
tap water which may contain residues of estrogen
from the birth control pill,
Estrogen in the food especially meat where the animals
are given growth hormone,
Hi David, yes, I’ve heard a lot of people say that and I too believe it’s about hormone imbalance. What did your wife do to balance the hormones? What did she cut out of her diet? What did she eat? Any advice appreciated!
You know how life goes – these things affect everyone differently. I eat a diet filled with greens and no hormone meats and my hormone levels were tested as balanced. I am so happy that your wife didn’t have to go through this and you guys have a beautiful baby. I am approaching 30 and I hope that I can be blessed with kiddos as well and soon. I am approaching 7 weeks post op now…this was my destiny and I was brought to and through it!
Lots of valuable lessons in going through this experience, for sure! I’m so much stronger than before. That’s the mystery of fibroids isn’t it? No one has any clue why they appear! Some people believe it is through stress or inherited trauma… who knows??
Really appreciated all of these comments – it is good to know I am not alone.
I am 3 weeks post-op, 5 fibroids removed with the largest baseball sized, bikini line cut over a pre-existing C-section scar. My recovery experience has had some negatives, which I only share because I wish I had known this in advance. I recommend you insist on staying at least two nights in the hospital. I was discharged after one night, which at first I was thrilled about. I have a 16 month old and he needed me and I him. But in hindsight, I was not ready to be around him – toddlers just demand too much and they are hard to deny. But the main reason I wish I had been in the hospital longer was that I was discharged without my surgeon noticing I had a hematoma forming under my incision. By day 5, my wound was leaking blood. I was told it was normal by the PA (via phone call and emailed photos). But by day 10, I was very swollen and painful with more blood leaking. This was because the pressure of the blood was causing wound dehiscion. I will spare you the details, but the surgeon finally saw me and and reopened my entire wound. I had to “wet-to-dry” pack my own open wound for 5 days before they would suture me up again. This experience, the discomfort was, well, unimaginable.
Other than staying in the hospital another day, I think much of my “complications” could have been avoided if 1) they had shaved me before the surgery. I do not know why they wouldn’t, but having public hair there means they can’t put on steri-strips over the sutures for additional support. So stupid. 2) for the original wound closure, they used surgical glue, not sutures. The glue is now gunked up in my re-closed wound and stuck in my (so stupid) public hair. The yanking of the glue-stuck pubic hair is painful, of all the pain, this is the dumbest pain.
Other than that, my advice would be to buy dresses, like mu-mus, because anything touching the area is painful. I thought I would be fine with baggy pj pants, but even that is irritating. The sutures I have are heavy-duty vinyl and get tugged by the fabric of underwear, pants, whatever.
Be prepared for a long recovery – I was way too optimistic (I am healthy, do the good things, avoid the bad things, etc.) but sometimes life throws you curveballs. This is not what I planned for, but hey, guess what, I am in the 5% with the complications. If you plan for the worst, when you get a speedy recovery, it will feel much more sweet. I did it the other way, and it is much more bitter. I am still so exhausted and in pain that I get panicky, but I think it is just PTSD from the hematoma/dehiscion. Luckily, I have a great partner and supportive family. Also, the pandemic means I can WFH and not use all my sick time. Silver linings…
Am I still glad I did this surgery? Yes, because I had to – because I want my son to have a sibling, because I love being pregnant and will love my future sweet baby. But this has not been easy, and I have a long way still to go.
Thank you all for sharing your experiences and fears and allowing me to share mine.
Hi Eve,
Thanks for sharing your experiences. Sorry that you’ve had to go through all of that and hope that you are on the mend now. I’m surprised they sent you home after a day! I definitely couldn’t have left the hospital that soon. I had my op on the Tuesday and left on the Friday – that was ok.
3 weeks is still early, so you are bound to still feel exhausted and still have some pain, especially after complications. Hopefully, in another week or two you’ll be feeling much better!
Sending love to you! x
Hi Helen,
Thank you so much for such a helpful post, by far the most informative source I have found. I am currently trying to decide whether to have an open myomectomy to remove a 12 cm x 10 cm x 8 cm fibroid. It has a small central area of degeneration but I’ve been very lucky (so far at least) not to feel any pain; I guess that could change in the future.
My background is that a couple of years ago a gynaecology consultant advised me and my partner that the fibroid wouldn’t affect our planned IVF but after unsuccessful treatment, our IVF clinic suggested we get a second opinion. The NHS consultant advised that the fibroid probably was causing the problem but recommended taking Esmya rather than having surgery (even though, like you, I thought Esmya had been suspended). We were a bit unsure about that advice (because of the Esmya risks) so arranged a private consultation, and the private consultant advised that the fibroid definitely wasn’t the problem but that she would be willing to remove it anyway as it would make any future pregnancy much easier. We have decided not to take the Esmya, but it’s not been easy deciding whether to have a myomectomy after receiving that conflicting advice.
We are trying to weigh up all the pros and cons of surgery so I wondered if you would mind saying how recovered you feel now its a year on from your surgery? Have your stomach muscles fully recovered and do you feel you can do everything you could have done before the pain began? Is there any residual numbness or pain? I swim quite a lot (or did in pre Covid days) and I can’t imagine ever being able to do a flip turn again after the surgery you’ve described!
Thank you again for your post, it really has been so helpful.
Best wishes
Jane
Hi Jane,
Glad you found it helpful.
I wouldn’t touch Esmya again personally. And it didn’t work for me.
A year on, I feel so much better. I trained as a yoga teacher last June – 2.5 months after surgery. Possibly a bit soon as it was hard at first but after 3 – 4 months I was soo much better.
My stomach feels fine. My core is still a bit weaker, but I feel like I can do everything I did before and more. There’s no numbness or pain now. And don’t see why you wouldn’t be able to do a flip turn in the pool. The problem is more stretching the other way at first, backbend not folding forward.
Hope that helps!
Helen
Thank you, that is really helpful and I also really appreciate your kindness in giving advice so long after your surgery. I think I will go ahead. Thank you!
Hi Helen and everyone!!!
Thanks for this elaborate post and the comments. I am scheduled for a surgery on Tuesday. Thanks for the information on what to pack and what to wear. I am positive for both the surgery and post op recovery. My doctor said it will be a cosmetic (bikini) cut.
I will come back here to share my experience.
Hi Karen,
I hope the surgery went well!
Let us know how you got on! x
My sister had surgery to remove uterine Fibroids on Thursday April 1, 2021. She stay overnight at the hospital and the hospital released her Friday Morning April 2, 2021. She was in pain but by Easter Sunday, she felt better after taking pain medicine. The morning after her surgery, the doctor who performed the surgery informed her that she would have to have another surgery, as there was not enough material left during the first surgery because the Fibroids were so big that they ran out of material. They told her that they were the biggest that they had ever seen supposedly. On Tuesday April 20, 2021, my sister had surgery to remove the remaining fibroids but although the surgery was completed, there was a three-hour delay. She was sent back home the next day just as she was after the first surgery. She said that she was not in the same pain that she was in from the first surgery but she did say that she felt dizzy and felt like she was about the throw up when she was still at the hospital. We talked to her a few times when she was back home and she called as well. She told her son that she was in pain but not as bad before and I texted her about 9:08pm that night and she told me that she was sleeping. The next day we called her but could not contact her. Eventually we went to her apartment and she would not answer. We got law enforcement to open her apartment door. She was found deceased in her bed. She was on her stomach and she appeared as if she was sleeping. The coroner said that she died from a blood clot that went to her brain but the coroner convinced my mother not to get an autopsy. I do not know if she was taking anti-blood clot medicine or if they had her wearing stockings. We have a lawyer discussing the situation now. DVT is a risk with this particular surgery but things do not make sense as to why she was allowed to have the surgery so soon after just having the other one because supposedly it takes 4-6 weeks to recover from the surgery. Also in the hospital, she mentioned that her blood pressure was through the roof. My sister had a history of seizures and high blood pressure as well. Her blood pressure medicine never really seem to keep her blood pressure in check. I just wonder should she even had the surgery with her health problems. Were the doctors aware of this or did they even care? The hospital that performed the surgery recently was sue for malpractice and my sister told my mother after the surgery that one nurse did not appear to know what they were doing and didn’t have the pain pump available until another nurse arrived and knew what to do. The Autopsy said that her death was the result of probably Pulmonary Embolism. Secondary factors were obesity, hypertension, and recent surgery. Please be careful.
I’m so sorry to hear about your sister. With any surgery, complications can arise, however, this sounds like a case of complete incompetency by the doctors/staff/hospital involved and very rare indeed.
What country was the operation in? What hospital?
I really hope you get justice for your sister. Thinking of you and your family.
Thank you so very much for your concern. My family are mostly made up of Africans Americans and we live in America. My sister received her surgery from hospital called Greenville Memorial Hospital. My sister was clinically obese but she was not massive just thick but she did work at Michelin for 12 hours a day (2010–2021) besides her normal days off. She definitely took blood pressure medicine but it did not appear that she could ever keep it in check because it was abnormally high even when she taking the medicine. In fact, the morning after the surgery she complain to us that her blood pressure was through the roof. In addition, she was experiencing Seizures that begin to happen in 2017 but I remember many years before she had an event that seem to be a seizure. Her son actually recorded a seizure she had one day and it was terrible to see. I could never truly get my sister to take it seriously, as she never wanted to believe she had these problems. She had one event where she had a seizure while she was driving and crashed her vehicle. One seizure event happen while she was walking to her car leaving from work. That even lead to her staying at the hospital that very night into the early morning and she was out of work for six months. Because the doctors could never induced a seizure she was never diagnosed as being epileptic but she took medicine for it however she wouldn’t always take it as prescribed. My sister was 43 years old. She did not smoke but she would occasionally have a beer. Sometime I believe in late March or April before the first surgery she had complain of chest pains while she was washing her clothes at a washing clothes store. She called my mom and said that her chest was hurting but it resolved on its own and she had believed that she might had pulled a muscle. My mom and she did not tell me what type of surgery it was that she was having so I did not really know about it until the first surgery. When I look about Myomectomy online, they did say there was a risk of DVT causing pulmonary embolism so I would hope that if her surgeon knew about her high blood pressure, seizures, and obesity they would have had her taking anti-blood clot medicine and wearing stockings. Thank you so very much for your concern. Always have people around you who love and care for you. Peace & Love.
My experience started about 5 years ago or more when I had heavy periods and needed one removing that was hanging in the middle of my womb, at the time it solved the problem.
Seems hereditary for me as my mother suffered with them and it ended in a hysterectomy.
Fast forward to about three years and I began to feel pressure on my bladder and could be uncomfortable after sex in the bladder area. Much to the dismay of my at the time, selfish, unsympathetic partner who ended our relationship.
Good riddance, ladies if you find a decent man keep a tight grip ! they are hard to come by.
Long story short after waiting for scans and a consultant I needed three large ones to be removed, biggest being 72 x 52mm so not as bad as some.
Out of the three options given , a myomectomy seemed although the most extreme option, the most sensible one as they would be removed.
Being in the wall of the womb was the problem, so the two in the wall were removed and they managed to remove the one in the womb going in through my cut.
They also removed another seven that were in the way of the three that needed removing so just as well.
I also had zoladex injections three months prior whilst waiting, to shrink them, I had to stop having them as they didn’t agree with my joints and my elbows still aren’t right. Because of the long wait for surgery, I was lucky my family paid for me to go private .
I lost a litre of blood during surgery as apparently I bleed a lot, so that didn’t really help.
Waking from the operation, I was hooked up to an IV drip, morphine drip, temperature disc stuck to my head, legs attached with inflatables, oxygen mask, catheter, stomach tube to drain blood and my arm being inflated every half hour to check blood pressure. I think it’s best to expect the above (hopefully not the blood loss) although must say my ignorance to it all beforehand was bliss.
The first night is the hardest, the morphine will dull the pain but won’t totally eliminate it.
Like others say take it easy, rest, eat well, sod the house work and accept help from others.
Must say although you don’t always feel like it, walking is a big key to recovery. I started at 5/10 mins a day and now I can be at 30 – 40 mins to not push it.
Do the exercises they give you as soon as you feel able but gently, don’t push it.
Sometimes when I was walking my stomach felt so heavy and there was a pulling / dragging down sensation which seems to be normal, that’s stopped now.
Generally just listen to your body.
I’m now six weeks since my op, everyone’s different but I have already started driving but not every day.
I definitely felt it in my stomach muscles and stomach area would get more tender.
Im working part time this week, day on, day off for three days. Not driving on my day off.
Seems to be the right way for me so far easing into it.
Might be a bit pre but I cannot fit into my denim shorts although I’ve actually lost weight.
I’m still getting very bloated, my stomach often feels heavy and since surgery I have a little spare tyre above my scar line which I’m hoping will flatten in time, I’m also still numb above my scar, scar area and the scar feels tight across my stomach.
Just be prepared for things to take time, it can be frustrating.
Little by little I’m improving and the nurses said realistically it will take three months and no heavy lifting for that period.
Hopefully the op will all be worth it in the end and I’ll feel the benefits more as time goes by – me being impatient.
Although it might now be too late being in my 40’s I still have my womb but was told I would have to have an early caesarean if I got pregnant.
Part of me is hoping for early menopause as I’ve had my fill of problems over the years with these space invaders.
Just thought I’d share and also wondered when the bloating / heavyness is likely to subside from other peoples experience.
If there’s anything I can do to help this side of things?
Hi Holly,
Thank you for being so brave and sharing your experiences with us.
The bloating goes down at different times for everyone, but usually after a couple of months I’d say! Hope you are back to 100% soon! xx
Wow, Having my surgery in two days and I am glad I found this blog. We truly are warrior women.
Glad you are finding it helpful! 🙂 We truly are.
thank you so much I just had my myomectomy June 25th and I found your article a week before my date and your article helped me out ALOT. I feel like ur experience was the same as mine
I’m so glad it helped! Here’s to a speedy recovery for you! xxx
Thank you so much. I’m 2 weeks post laparoscopic myomectomy and even though my operation was a much milder version than yours I found it helpful to read your story. I too have felt the involuntary stretches the first 4-5 days post-op and again this night. It might be the anaesthetics as you say. But I also have a theory that it’s my psoas muscle. The Psoas is very sensitive to stress, chok and anxiety and an operation is indeed a traumatic event for uor bodies. Also the fibroids have been putting a lot of stress on the system for years and suddenly getting rid of that stressor might also be what makes the psoas want the whole body to stretch out and feel the new sensations. When I’m ready I’m going to do a TRE (Trauma Release Exercise) for myself to shake the trauma out of my body just like animals do.
I can also relate to the anxiety seeing the wounds and stitchesfor the first time. I have 5 incisions and the biggest in my belly button and I was totally freaking out when I had to remove my band aids A friend of mine did some healing on that and uncovered a past life trauma that needed healing. After that I’ve had no problem looking at my stitches.
I read in the other comments that yor asked a guy what foods his wife/girlfriend had been eating to get rid of her fibroids. I too have been doing a lot food wise in order to shrink my fibroid. It was just too big when I started my protocols. But I firmly believe that my eating has been why I’ve only grown one large fibroid over the course of 11 years. Also the fibroid was nearly calcified when I finally had it removed and the surgeon didn’t see any signs of small fibroids while operating. I’ve been eating mostly antiinflammatory foods and for a period I tried the Medical Medium diet but with no luck. Actually the times I’ve felt the fibroid grow the most have been during very stressfull times where I didn’t take good care of myself and ate lots of dairy products and sugar. Since last Christmas I’ve been detoxing the part of estrogen called estradiol using a very clean chlorella product, milk thistle and lots of vitamin C. After the detox I began using bioidentical progesterone cream also to balance my hormones. In the fall I’m going to a Natural Hormone Therapist to start a protocol so I will never grow fibroids again. Anyway I believe everything I’ve done on my own thus far have definately helped stop the growth and make my fibroid almost turn into a fossil
Also the last couple of months I’ve been doing a lot of EFT tapping on all the feelings I had around having a fibroid. This has been an eye opener to me. I feel like I’ve used this fibroid as an air-raid shelter protecting my inner child from all kinds of emotional issues. I’m now taking care of me and I want to stay on this path of being true and caring to myself.
Again thank you for sharing your story and I hope you find my experiences usefull ☺️
The psoas releasing! Of course! My right size psoas is so tight and I am stretching all the time, too. My fibroid was more on my right side. My hip flexors and psoas feel the most affected by this surgery.
Milk Thistle is my plan for this coming week to detox all the painkillers. I keep getting headaches. My liver needs some support. I am not eating that differently. My belief is that my fibroid was my grief baby. I didn’t have children and I was so sad but felt completely powerless about the situation from 42-47. I was so distraught about not figuring it out I let myself be celibate for 6 years. Also, I had a huge falling out with a dear friend, moved countries, went into debt, let go of my yoga teaching career. I also stopped practicing (more or less) due to disappoint in myself. My 40’s kinda sucked.
My 49/50th year, I got diagnosed with ADHD which has massively helped me forgive myself, fell in love for the first time in 10 years, with a man 15 years younger who is the best boyfriend of my life. Huge growth period for me and the fibroid grew a lot as well.
I think a lot of energy moved that was deeply stuck and held, cycled rapidly and demanded to be released. It had to be through the fibroid and surgery but that’s ok. I feel released and free now.
Hi Helen,
You were so kind when I commented above that I thought I would come back and let you know how I got on. I had my surgery on 30 June and although my blood pressure dropped a lot during surgery and afterwards, otherwise everything went well and I was discharged after 48 hours. Being back at home is lovely and I’m now resting as much as possible, and getting stronger each day. I would not have gone in at all had it not been for your post, and I would not have been even as quarter as prepared without your advice so I am deeply thankful to you.
In return I hope I can contribute to your thoughts on changes to prevent recurrence. Before I went into hospital, I read a lot of research papers about non-surgical treatments for fibroids, especially reaseach into natural compounds that occur in foods. I have no medical training whatsoever but I know conventional medical wisdon is that fibroids grow in the presence of oestrogen and progesterone so they can recur at any time before the menopause. I have two small fibroids as well as the large one that was cut out, and I didn’t want them to grow once the large one had gone. I was interested in natural compounds because drugs like Esmya are really not a satisfactory option.
I can send you the links to the most useful research papers if you’d like to see them but I think the most promising treatment at the moment seems to come from a compound in green tea. I found a few studies and they all showed a reduction in fibroid size when this compound (EGCG) was taken. They were small scale studies and the participants started with small fibroids but it looks really hopeful. Obviously it wouldn’t be a replacement for surgery for large fibroids but it could stop smaller fibroids becoming a problem.
There was also a really interesting paper collating earlier research into lots of different foods. That suggested a correlation between having fibroids and a higher meat consumption, dairy consumption and fish consumption. However, it seemed like the link possibly could be due to pollutants in the food. (There’s a similar BPA link in animal studies.) There is also research showing a correlation between fibroids and vitamin D3 deficiency. On the other side, there is a correlation between having fewer fibroids and a higher fruit and vegetable consumption. Almost all of the research concluded that more research was needed, which I would definitely agree with!
I can become very boring on this topic so I’ll stop there. Let me know if you’d like any of the links, I seem to have a small library of pdfs now.
Thank you again for your post and for sharing your experience.
Dear Helen and all your commentators,
Thank you, thank you, thank you for posting this! I am Day 6 post-op and have been having the most terrible pain which I now recognise as gas(!!) so I am pepperminted to the max and feel much better already. I found this article after despairing that there is so little detailed info about post-op recovery and was desperately searching to see whether anyone had written anything dealing with quite how I have been feeling the last few days.
Thankfully the op itself went smoothly for me – and I am in awe at what some of you lovely ladies have been through. Hope everyone is recovering nicely now.
Much love xxx
Hi Helen. Thanks so much for your blog. I’ve been feeling a bit down as I have an open myomectomy coming up and I read that one woman could no longer do headstands or inversions more than 3 years after doing the surgery. I was wonder how you are finding doing yoga poses, in particular inversions and if are able to do them yet? Thanks so much, D
Hi Denise,
I could never do inversions anyway, but I wouldn’t worry too much. Everyone is different and many people can still do them. Don’t push yourself though. Good luck for the op and sending positive vibes your way! x
Hi,
Wow what a wonderful read on fibroids, there really isn’t enough information on the web about them .
I am 40 with no children and have been diagnosed having multiple fibroids, largest one being 12cm.
I am really unsure on having the surgery, partly because I am very worried that something will go wrong and they will have to remove my womb, I would love to have children but its sadly never happened for me, the thought of my womb being removed fills me with dread. I would not be able to cope with that mentally. So for that reason I have decided against the surgery and I will carry on living with the fibroids. I don’t suffer with heavy periods, I just have a very bloated stomach and I had a degenerated fibroid (which was very painful, that alerted me to find out that I had them otherwise I would have been none the wiser)
I know this isn’t the correct thing to do but I cant help thinking that the worse will happen.
Did anyone else have these thoughts?
Hi Tasha,
When you meet your consultant, they will always give you the worst outcomes possible. I would ask lots of questions when you go to the specialist. Ask to see the scan, ask where it is located and what that means for you. I was offered some Gonadotropin releasing hormone injections which reduce the size and puts you into menopause. It maybe worth exploring for you. However , this means the fiborid would lose definition and might make it difficult to remove. I turned it down because with COVID, i wasnt sure when i would have the operation. I was like you, had not had children and delayed for years as I didnt want to risk losing my womb ,as I was managing to cope with the symptoms. However, because mine were multiple , of various sizes, i was more at risk of a hysteroctomy, but they were impacting my health and everyday life: so my health came first. The thing with fibroids is: they dont go away and tend to multiply.
It is daunting , knowing you may risk the very thing that makes you a woman, but you have to weigh that against your quality of life as time goes by. Ultimately, the decision is always yours to make.
Hi everyone,
For those of you who had an open myomectomy, could you pls let me know when your belly came back to normal?
It has been almost a month now since my op and my belly is still very big and swollen-just a bit less than pre-op. I read many comments about similar experiences but I’m worried and I’m wondering how long you all had to wait for your belly to go back to normal… Did you do anything to shrink its volume?
Any comments appreciated!
Tx
Hi Robbie,
The belly is a struggle indeed. I think it is based on the individual. I am 7 weeks post op and mine is still there but not as big as it was. I have decided to concentrate on the physiotherapy side of things to strengthen my abdominal muscles and also my back before I start doing any exercise. Listen to your body. https://www.rcog.org.uk/en/patients/patient-leaflets/recovering-well-from-gynaecological-procedures/
This is a good one for just getting some strength back and also making sure your back stays strong. I didnt realise until i started doing the exercises just how weak my abdominal muscles had become!
Thanks
KR
Helen and all those who have commented and shared your stories. I just wanted to say a HUGE THANK YOU. I am now nearly 5 months post op and there is no way I would have gone through with it if I had not found and read all your comments here. I was petrified and reading your stories was both a balm and fortifying and gave me a realistic idea of what to expect. None of it has been easy, mentally or physically but it has been worth it. I feel stronger in so many ways since my op, it was certainly the right decision for me. Thank you Helen and all of you. Love and strength to you all. xx
Just wanted to leave a big thank you and send you and every woman dealing with these fibroids a warm cyber hug. My surgery is in 3 weeks and I’m scared but feel a little better having read your blog. I’m 37 with no children, with a 10cm fibroid along with two smaller ones, having an open myectomy at the VA hospital. Blessings.
Thank you so much for sharing your experience, and doing so in such detail! I have an open myomectomy scheduled in 3 weeks, and am praying I will be able to have the surgery. Hospitals where I live are overwhelmed with COVID patients, so “elective” surgeries that require overnight stays are being pushed back. In any case, it sounds like I’m dealing with a fibroid close to the size of your large one, along with at least one other smaller one. Anyway, this helped my anxiety SO much! Just having an honest account of what to expect is wonderful – and the packing list for my hospital bag was a huge help. You’ve helped many, many people by sharing your personal story. I am one of them and I am grateful.
Hi Helen,
I enjoyed your story, and am glad your end result was so promising. I had an opposite experience. My myomectomy was botched, and I will go so far as to say my life as I knew it ended that day–April 25, 2016.
I had Stage IV endometriosis and had already had a laparoscopic procedure for it. My doctor “unglued” my ovaries from my uterus, and my uterus from my tubes, but did not have time to get to the fibroids. I moved to California from Mississippi three weeks later, and thought I’d just live with the fibroids. After sweating out the pain from endometriosis for three years, I went to another doctor when I moved home who had been referred to me by a co-worker, RED FLAG. I was too scared to go back to the doctor who did not “have time” to cut out my fibroids, and my co-worker actually knew him and said he was a “butcher.” Little did I knw that the doctor she referred me to knew NOTHING about endometriosis and simply wanted money. I have since found out she botched four other women, leaving them sterile as she did me. In a nutshell: My inexperienced myomectomy surgeon was just a plain OBGYN. She scheduled major open surgery the same day she met me. I wanted the pain to stop and trusted her (we trust doctors but shouldn’t–they are falliable humans who ruin lives every day). She over-operated, TAKING MY LEFT FALLOPIAN TUBE WITHOUT PERMISSION. She removed 11 fibroids (I did not want them all removed, just the big ones). I needed a blood transfusion but refused, because she did not warn me that I would need one. She told me about NONE of the risks, only that any pregnancies would have to end in C-section. She scarred my uterus to the point that I did not get to have children, and I also do not get a period anymore due to losing my tube. (It had a freak effect on my hormones) I wish I could go back in time, because I would take endometriosis and 100,000 fibroids back just to be whole again. I have aged rapidly, quit being social, no longer date, and have to live knowing I was sterilized by a money-hungry idiot who basically used something other than books to graduate from medical school. She also yelled at me to “get up and move around” and didn’t even REMEMBER ME at the follow-up appointment She also said she saw “no signs” of my endometriosis, because I WAS NOT ON MY PERIOD DURING THE SURGERY!!!! On the way of the room at my follow-up, she rudely told me to “get a hysterectomy.” I requested the op report two years after my surgery, because I wanted to see what she did. My life was falling apart. She put on the report that I requested my tube be removed! She also put I had a laparascopy, not an open surgery , did not mention the 11 fibroids, and there were no pictures taken. I would have done better getting the surgery done in a back alley. I checked with lawyers who said, “After two years, you can’t sue, no matter what she did.” I also found out doctors here in Mississippi pay off the courts to avoid malpractice suits anyway. I now have to see an oncologist surgeon to deal with the issues she left behind. My pubic region feels like a rock, and I have no range of motion. I am a former athlete, so you know that’s bad. This sounds terrible, but I wish I had never woken up from the surgery knowing what I’ve been through because I stayed alive. I really am glad to know others have not gone through this. I used to have periods that left me crawling on the floor. I would do anything to be like that and not like this. Take care, and thank you for your story. — Hollie
Hi Hollie, I’m so sorry to hear about your experience.
That’s crazy that you can have doctors like that in the USA and that you can’t do anything about it? I’m so sorry you had to go through that.
Sending you lots of love.
Hello!
Thank you for sharing your story reading this was very helpful and gave me hope that I will be better soon! I am currently recovering from a Myomectomy surgery that I had on September 15th. My pain level is around a 3-4 and I am now walking a bit more than I could the day I was discharged from the hospital. My experience was similar to yours, I also have a vertical incision below my belly button. Before all this happened I had experienced a DVT in my left leg and this was all due to the fibroid so if you do have a fibroid that is bothering you and you are reading this don’t wait too long. My fibroid was about 15cm and was sitting on a vein in my leg which caused me to have blood clots. Thankfully I went to the ER and was given treatment for three months to get rid of the clotting before my surgery. In those three months my fibroid grew from 15cm to 19cm! So please don’t wait listen to your body and if your doctor recommends surgery don’t hesitate! I was treated at UCLA hospital and they did a great job! According to my gyno My surgery was hard but I had no complications and I was able to go home and rest after two nights in hospital. I am super happy now that this thing is out and I can finally recover and be myself again!
Hey Helen..so brave of you to face the procedure and so thoughtful to pen it down.My fibroid is also large like yours but it is asymptomatic except for the bulging tummy.I am also contemplating surgery and I get chills in spine to think of it.I am also exploring other options like uterine artery embization but at this stage it is only r and d.
Hi Shweta, I hope you get it sorted soon! The surgery wasn’t as bad as I thought it would be and I have no regrets about doing it! xxx
Thank you for sharing your journey Helen. Much appreciated as I am due for the same surgery next week.
Hi Sandra, I hope the surgery went well! x
Hi Helen,
Thanks:-). It went well, save for the chest infection I got on the day of discharge, that was painful but thankfully cleared now. Just now starting light physio and walking correctly. Much harder than I thought.
How did you sleep post op during recovery as that is my current challenge? I can’t get comfortable at night. One side is more painful than the other. So, I end up sleeping up or on one side.
Hi Sandra, I slept on my back, but piled pillows up beside me so I could rest my head to the side (as I prefer sleeping on my side to my back)! 🙂 Hope that helps!!
Thanks will try.
Hi, Helen..
I’m sitting here, exhausted due to being anaemic as a result of fibroids causing heavy periods. I’ve dealt with the symptoms with tranaxemic acid (it works but it’s not enough and the blood clots as a result are huge) and iron tablets (3 a day when I was at my lowest) and regular blood tests to monitor my iron levels, but as it gets better it gets worse again. I don’t want to be on tablets forever. My exhaustion stems back years, but at the beginning I didn’t know the cause and thought it could be something much worse. I couldn’t even walk the 10 minutes to work without feeling like I would collapse.
Finally with my doctor referring me for blood tests and calling me demanding I go back to the hospital in the time it took me back home, I was diagnosed. I have a weak bladder I think due to my womb pushing on it, I have sciatica due to I think everything pushing on my sciatic nerve. I’m just so tired, I feel like my life is on hold. Every time I look at treatment it’s overwhelming as there is so much information. I”m so happy that I found your post and your personal story about overcoming this.
I have a doctor’s appointment in 2 weeks and I’m determined to get a solution and my life back.
Hi Leah, I know the feeling – it’s horrible.
I don’t regret my surgery one little bit! 🙂
I hope you get everything sorted soon! xx
Hi ladies,
Just wondered how you slept after the operation when back at home? Especially
after an open myomectomy? I can only sleep on one side as the other side is painful. But have broken sleep as I get uncomfortable sleeping in just one position.
Before hand, I used to also sleep on my front.
Thanks
Thank you Helen and all the women on this thread. You’ve made me feel like there’s a level of hope and clarity that my doctors haven’t given me. My fibroids have been an incredibly isolating experience and it’s just so wonderful to hear so many of your stories, with all their scars and rough edges.
I’m in a pre-surgery waiting game. I’m 31, and we’ve been monitoring fibroids since 2019. In September I got into a car wreck, and the CT scan showed they’ve grown massively. Now I have a 11cm right one, a 10 cm left one that buldges out after I lost my pandemic pudge, and two smaller ones. I’m frustrated that the doctors had me wait and see until they got too big to do anything but an open surgery, but here we are. I’ve got a hieretary clotting disorder so I already had awful periods. They’ve gotten worse, but now I can’t get tampons or menstural cups in, and the last month it’s constantly felt like something is falling out of my vagina from the pressure. My left one is sitting on my bladder, and the right has divated my cervix. I want them out to and to be moving forward, but our hospital system in my city (US based) is a mess with a nursing shortage so they’ve had to constantly delay and the soonest they can get me in is April. We might be able to do it in my partner’s home city near his parents this winter, but we’re in a battle with insurance to make that feasible. I know I’m in the same boat as a lot of people with this pandemic but it all just feels like life is on this perpetual standstill.
My doctor said it’s a 50/50 whether they would do a vertical cut or just a bikini, and likely won’t make that call until I’m already under on the operating room table because they need to evaluate it under anesthesia. That part scares me a lot, just the not knowing what I’m going to wake up to. I guess if I prep for the vertical I can only be pleasantly surprised if they don’t. I’m also worried about the pain management. I had kidney stones removed in 2016 which everyone promised would be easy peasy until I ended up in a pain spiral and back in the hospital for 4 nights. But I’m hopeful my medical team can bring some lessons learned from that experience. Turns out I don’t tolerate opioids at all so having a well built alternative plan will be really critical. And I’m really sad about not being able to pick up my 16-pound jack russel for a while. But I’m hoping this ultimately releaves a lot of health issues and mental stress and lets me get back to a full life. Fingers crossed we win the battle against the big insurance companies and make January happen!
Hi Helen,
Thanks for this wonderful article and for sharing your experiences. I’m a homeopath and wanted to let you and your readers know other useful remedies for your hospital bag and post- surgery.
I recommend using arnica 200c both the day before you go in and after and to carry on with it for a number of days after. I also have my patients make up a water bottle with 5 of the following pellets of each in it –
Bellis perrenis 30c (for deep organ bruising)
Hypericum 30c (incision healing)
Calendula 30c (scarring healing)
Staphisagria 30c (for pain after uterine surgery)
Post surgical gas can sometimes benefit from lycopodium 30c taken a few times as well.
Hope this is helpful!
Sue
Sue, thank you for your post, I’ll do just this
Hello,
Like everyone else I am looking for answers and doing research on my newly found diagnoses. I’m just in the beginning stages but I’ve been dealing with lower abdominal cramping, discomfort, pain, pressure, urine frequency and that discomfort feeling on the lower right back and on the sides of my stomach for the past couple of weeks.
After multiple test, panels ect no bacteria or yeast. However I was told I may have a prolapsed uterus. So my obgyn put in a referral for pelvic therapy. I was one day away from my ultrasound and ended up having to go to the hospital yesterday. I am 37 almost 38, single parent of an almost 6 yo boy delivered by c-sec.
At the ER they took blood and a transvaginal ultrasound (the vag wand) was done.
I was told I have an ovarian cyst on my left and frght side and a fibroid, but that was not the main reason I was there, I just wasn’t feeling well and had weird symptoms earlier like my body got warm quickly and I felt weak and shaky, I didn’t eat much so I thought it was my blood sugar, but I found myself hunched over the bed calling 911 because I knew I could not drive and I had my son with me.
While on the phone with my mom I was talking and then all of the sudden it was like I couldn’t finish my sentence and I felt like I couldn’t breathe I found myself on the ground hyperventilating and crying until emergency response could help me, I was so scared but my son was there and he was so brave about the situation. My body was stiff too like I couldn’t move it.
I guess my body had enough but later on I found out it could have been a panic attack or fainting spell. I’ve been mostly resting and taking it easy. The heating pad has been my best friend but I would’ve never known if I hadn’t come to the ER, now I’m just waiting to have my follow up appointment with my primary doctor on Friday and another follow up with my OBGYN next week.
I was supposed to be returning back to work this week but my body has other plans, I feel like I’ve been dealing with these kind of symptoms for years now but never got checked out, it was always a GI thing or a stomach bug. Also life keeps you busy and when your a parent your child comes first and our health gets to a point where we just manage the best we can but goes unchecked or misdiagnosed.
Reading this article and everyone else’s journey have been most helpful, though I’m not for sure how big my fibroid is but I did manage to make it to my other ultrasound appointment and it was a little different then the one at the ER so hopefully come Friday I have more answers and options for my issues which have been debilitating at times, stressful and exhausting.
And if not, I find that I have to advocate for myself and push to get imaging done because right now everything is backed up in the healthcare system and some doctors will avoid having imaging done due to various reasons so don’t be afraid ladies and get your needs met, thank you all.
Hi Helen,
This is one blog I kept coming back to before my surgery, which happened on 10th Feb. I am still in the process of recovery, but wanted to share my experience.
My fibroid was pretty much as big as yours. It was size of a cantaloupe. My surgeon took fairly dramatic pictures of fibroid, uterus etc. I wanted to keep my uterus and my surgeon promised that he would. It’s really important to find the right kind of surgeon. My doctor recommended a fertility specialist. They are more likely to respect a woman’s wishes of not removing the uterus. Others are not that careful. I got with my hunches when it comes to doctors. I met my doctor and was sure that I was is good hands. So, that really helped. They were really concerned about my blood reports. I have thalassemia trait and am a small number of people with thalassemia trait, who have severe iron deficiency. This got recently diagnosed. As luck would have it, I am also allergic to iron infusions. One of the hematologist at the doctor recommended it for me. I was not comfortable with the idea, but went ahead with her suggestions. I got an anaphylactic shock and almost died. They stopped the treatment and since then have primarily relied on iron supplements (thrice the recommended amount) and folic acid (helps with absorption of iron). Alright, back to after surgery. My surgery went off well. I was in the hospital for two nights. They did take the catheter out the next day. I got dizzy and it took me forever to pee. I thought I would never be able to do it. But, in the end it worked and it was not painful. Bowel movement was painful. I had my first one today, five days after the surgery. Stool softeners were causing bad side effects, so I didn’t take those. I tried climbing down the stairs yesterday and that was a bad idea. Other than that, I think I am recovering fine. I did have my periods a day after the surgery (I was due then). It was lighter than the previous one. Frankly, my period pain used to be something else (absolutely unbearable). It was bearable this time, probably because of all the pain killers. I did buy some loose underpants. This was thanks to you–a brilliant brilliant suggestion. I didn’t wear my own clothes in the hospital, but the underpants were so needed. Thank you for your blog!
For those who are planning on going through the experience, please don’t worry. I know it’s easy said than done. I was scared, but it’s much better to live without a cantaloupe size tumor pressing on your organs, giving you excruciating pain than to avoid a surgery. Here are few things to keep in mind. First, definitely find a surgeon, who also looks after women’s fertility issues. Second, even if you think you feel okay, don’t stress. Rest for the first two weeks. I am on day 5, but plan to rest for at least the next 7 days. Third, make sure you have good quality emotional and physical support with you for the first two weeks. Fourth, you can eat pretty much anything. For me, starchy food seems to help. I tried yogurt and it gave me massive nausea. Fifth, though they give your oxycodone, avoid it if you can. It does block your GI tract. I didn’t take any oxy. All the best! Thanks for the blog again, Helen! It’s my birthday is a few days and I am looking forward to it.
Hi Helen, thank you so much for sharing your story and tips! I had open myomectomy 3 weeks ago for the removal of 2 fybroids in my uterine wall. 6cm diameter and 2cm diameter. The results on the MRI came up looking a bit odd so the surgeon went with open instead of keyhole. Later found out the oddness was just a result of the larger fybroid degenerating and it wasn’t cancerous/precancerous. Surgery went well and in the process of recovery. I have a family commitment to fly to Hawaii at the end of April. This will be 2 months post op. The flight is more than 20 hours and I am a little concerned I will be putting my body under too much stress too soon. Also not sure if I’ll be able to join the family to do all the fun activities you would otherwise do there. How soon have others started hiking and swimming post op?
Thanks!
Another Helen
Hello ladies,
I posted a comment back in August 2021
I was against having the surgery as I over thought every possible scenario.
The fibroids started to bring me down, I sort of fell into a depression – I had zero energy and I could feel my confidence declining. I knew I had to bite the bullet and get them removed
After doing some research I found a surgeon who I warmed to (private) he understood my worries and concerns and put my mind at ease.
I am pleased to say I’m now 7 days post op, everything went very well.
He removed 17 fibroids (thought I had 9) the biggest was 15cm
The pain wasn’t half as bad as what I thought it would’ve been, the only time the pain got to me was when the physio came and got me out of bed the day after surgery, I got really emotional and regretted my decision, that thought lasted a matter of minutes.
Each day I can feel my body getting stronger and the pain getting less.
I’m going to have my stitches removed tomorrow, at first my surgeon wanted to perform a vertical scar but on the operating table he managed to do it via a c section (he’s a god)
I just want to say a huge thank you to everyone who has commented on this post but mostly to Helen for providing a place where us females are able to help one another out with our experiences.
it’s just so unfair that fibroids are not spoken about in this country, a lot of my family/friends did not even know about them.
I did come across a really helpful page on Instagram
@wecanwearwhite
Anyone who already has a date for “eviction day” I wish you every bit of love and support….. you’ve got this!!!!
xx
This blog and the comments page is the most comprehensive information on myomectomy I have found on the web. So let me add to the wisdom.
I am on day 13 post-surgery.
My first inclination that I had a fibroid was 2 years ago when I went for a routine Pap smear. The gynaecologist told me it was the size of a tangerine. But since I was 48, probably near menopause and it wasn’t bothering me that we could watch it.
From my newfound perspective: anything over 6cm, insist on removing it.
A year later I met a man. The sex was were the problems started. I would sometimes have great pain-free sex and other times I might experience 10 minutes of doubled over pain that could make me vomit. Often the pain was from orgasms, not always penetration.
I kept going back to the doctors to ask about the pain but no one seemed to be giving me good direction. 8 weeks ago I got totally fed up and went for a second opinion. The gynaecologist took literally a second to say ‘ That’s massive, it needs to come out and now.’
She told me it was posterior, which was going to be difficult. She said find the best surgeon you can as everyone else will insist on a hysterectomy.
I found a great surgeon in Madrid, as I live in Spain, who only does fibroids. She initially suggested a hysterectomy as one of my ovaries and Fallopian tube looked enlarged on her preliminary scan. Basically, the medical system, if you aren’t having babies they ‘suggest’ a hysterectomy as you aren’t ‘using’ those organs. Though I am 50 I wanted to keep my ovaries and uterus. Ovaries are part of the endocrine system and pump out hormones we need into our 70’s. I need my uterus and cervix for my sex life.
Luckily, my CA125 test, which is a pre-cancer screen was low scoring which indicated negligible chance of cancer. MRI showed my ovaries where fine.
The hysterectomy is also ‘preventative’ for cancer. I don’t have cancer on either side of my family so decided I am willing to take the risk and deal with it ‘situationally’ instead.
I had never had surgery and was very nervous. The two days before surgery I found myself walking 10 km a day and doing strong yoga, backbends and was in a handstand an hour before surgery. Celebrating and enjoying the freedom, the strength and lack of pain in my body for what would be the last time for a while.
I had an open myomectomy, bikini cut. The operation was a total success. No blood transfusion, only an hour, pulled out a 11x9x7cm or a babies head sized fibroid. They took pictures for me. Seeing the photo completely affirmed for me that surgery was the right decision. How had I lived with that in my body? What impacts was it having?
My brother nicknamed it ‘Cantanope’, my best male friend called it ‘Roast’ and my boyfriend kept showing everyone. Men.
Immediately, first thing I noticed post surgery is that the pain was less than what I thought it would be. Secondly I noticed that my chronically swollen right ankle and varicose vein were negligible and continue to be so. The lack of severe pain has continued to be the case. There is dull discomfort, pinching, sharp, uncomfortable twinges, fullness, weakness, soreness but a doubled over pain? Never. The worst pain has been from the UTI I got two days ago. And from the gas.
I am struggling not to overdo it.
Day 4 I went to The Prado and was pushed around in a wheelchair and walked a bit. My surgeon hit the roof when I told her but my 5 day scan showed no damage.
I seem to walk about 1800 steps a day on my walks.
My healing feels slower than I thought. My activity levels aren’t increasing yet. The scar pulls and tweaks still. I still haven’t figured out how to get up from lying down. That is seriously the most difficult part.
On the good side, the scar looks great, I have had zero complications, no cancer showed up anywhere, I have all my bits and I can feel my core re-engaging already.
I am a chef and I am sure I will need the full six weeks to get back to work.
Yoga consists of hero pose and arm stretches.
The harder part than the pain for me is the psychological part. I have ADHD and the lack of ‘busy-ness’ that used to dissipate my hyperactivity has now meant that my poor brain has had to run some marathons. My father said, ‘ why aren’t you meditating?’ But between the pain, and the boredom my brain says a hard ‘no’ for now. There is also contending with mental fog, struggling to find words !? vulnerability, feeling ‘old’, fatigued.
On a good note. I am also loving the lack of busy. Starting to get used to it. Catching up on sewing, taking a much deeper dive into how to use my Tarot cards, going through 10 years of papers that need re-organizing and/or throwing out. Napping. I am actually really looking forward to this next month of chill out
To finish: no regrets. On with the healing.
To add: I am 50, not in great shape as I rarely exercise. I used to teach yoga hence the handstand and backbends but I have only practiced a handful of times in a year. I have an active job. I don’t drink or smoke. This experience has brought me back to yoga. My agility and strength and balance are residual and I cannot wait to deep dive into reconnecting myself to my practice.
It’s actually exciting not frustrating as it’s like a ‘new body’ to experience. I will learn so much.
Hi Helen
Thank you for this article I’m so glad I found it. I go in on Wednesday 1st June to have an open Myomectomy pending hysterectomy but won’t know until they go in. I have a 30cm fibroid on the outside of my uterus and a 14cm one. I look full term pregnant.
It grew from being pregnant which was a miracle (being pregnant not the fibroid)
My baby is 4months old now and healthy all though being stuck under a fibroid the size of a basketball made the pregnancy very high risk and rare.
Your tips on what to pack are great and the outcome of your procedure gives me hope.
Xx
First, I would like to give a massive credit to Helen, for creating this space and shared hew story about fibroids. I didn’t come across to anything similar on this subject and was so relieved and glad to know that I am not alone.
Secondly, I would like to thank all women here who also opened up and shared their experiences. This is valuable information for those who are yet to step on the journey of operation and recovery!
My story began long ago, when I my gynaecologist discovered a 2mm fibroid, but said nothing to worry about. Several years later, my fibroid grew to melon size and wad severely sticking out of my belly, so some could say I looked pregnant. Luckily, I didn’t have any symptoms, apart of pressure to my internal organs and discomfort during sex and some of the exercises. This was the point when I agreed to operation. NHS was pushing for it, so I started to research and found one of the best doctors in UK, doctor Justin Clark in Birmingham Woman’s Hospital (if someone is local and looking for a good doctor, I would definitely recommend). He did all possible to prevent from any complications, but also suggested to remove it asap so I don’t loose the uterus later on. I just turned 33, when I had my operation and today I am 6 weeks post op. and ladies – it was the BEST decision that I have made.
My operation went smooth, quick and with no blood loss. The doctor were also able to perform a bikini cut (he is magician, as all other doctors (I have consulted with few privately) said they can only do vertical cut)). I was devastated when they have mentioned vertical cut. When I woke up after my surgery, they said it was low bikini cut and they only removed 1 fibroid, but for some reason nowhere was confirmed the size of it.
My recovery is going so well, that I couldn’t even imagine. it’s 6 weeks mark now and I am back to my normal daily activities (and I am very active person), dancing (amateur), running, doing yoga every day, walking etc. I have not been to gym yet, but I know I am getting stronger and stronger every day, as I am able to do plank, and abs work now.
My suggestion to those women who are waiting for operation – be very active few weeks before op, eat well, avoid alcohol. I also excluded all nuts, dairy and coffee products a week before op to prepare my stomach. After surgery I was able to eat normal on the second day (first day I was sleeping off my anaesthesia). I was out of bad on the second day and was able to shower even. First few days up to a week was difficult to get out of bad, but I could do stairs easily.
I have my post op appointment in few months only and I have also booked for a scan to make sure everything is healing well.
Oh, I forgot to mention that I was also on a prostap (injections that cause artificial menopause) for a year to shrink fibroid (needless to say that my fibroid didn’t even think to shrink 🙂 but at least it didn’t grew bigger. Being on prostap for such a long time I needed to take HRT (hormone replacement therapy) to prevent bone density. I am soooo glad and relieved to not be taking any of these. I didn’t have my period yet, but I am expecting it in the next few months. (as it takes time for ovaries to “wake up”).
Overall, it was great exoperience, not only physically but also mentally, as it takes a lot to prepare and go for something unknown (never know what you will wake up to). But staying positive and mentally encouraging yourself that everything is well and there are no other way- makes such a big difference.
I send a big warm hugs to all those who are in the waiting process – you are strong and you will get over this quicker then you know!
WOMEN POWER!!!!
Thank you for sharing your story in such detail…I’m afraid and preparing for surgery in a couple of days. This is tremendously helpful while in preparing and dealing with anxiety.
Hi helen
Happy that you recovered from this after all these struggles.. reading out your stories gave me tears as well as confidence too.
Im having my second surgery next week 11th august. Hope it goes well.
In february 2020 i got diagonised with fibroids in three places. Omg i never ever experienced this much pain in my entire life. Everytime i am on due for my periods i used to take off from work.. used to stress a lot.. because no painkillers nothing helped.
It was during lockdown so no doctors to see.
Finally august 2020 i got a date of ultrasound scan then i came to know this was because i had 3 fibroids.
Admitted in hospital few many times. They used to send me home . But pain didnt subside.
I even felt negative at times.
Then after two years in 2022 april they called me for a surgery. By this time my husband left me as he couldnt wait for having a normal sexual life and a baby. They did hysteroscopy keyhole surgery when i woke up from anesthesia doctor he could see any fibroids . So they didnt remove. I started crying. Then why am i getting this much pain.
After the surgery i was discharged had a follow up their i cried a lot then they agreed for open myomectamy .. i got infected after my first surgery .
Hope this surgery goes good. Bit nervous .
Trying to be positive.
Men like my husband should realise women is not a sex toy or just for giving baby..
Abarna!
I just read your story.
How are you feeling now? Are you feeling better? How was your surgery?
I’m sorry about what happened to you! It is very unfair, and unfortunate that that had to happen! I hope you’re doing better now, feeling better now, and I wish for you for the best that you’ve ever had!
<3
Hi Helen
Many Thanks for bravely sharing your fibroid story with us. I recently learned that I have them too – I don’t know the specifics yet, but I had the ultrasound and yep! They’re there. I have a follow up with my OBGYN to discuss further treatments, and what’s next.
Honestly, I’m super freaked out. I have history of cancer and can’t helped you think that this is associated with it.
Reading your story helped and reminded me of some things I went through during my first cancer surgery.
But, I just want to say many thanks! Knowing that there are others that can relate to what I’m going through is something and that there is a light at the end of the the tunnel.
Thank you so much for sharing your experience. In recovery at the moment and you’ve helped me a lot!
Thank you so much for sharing your story. I have multiple fibroids and need to get operated soon due to their size and the fact that I was in the ER last week due to one of the fibroids degenerating. I will be discussing with my gynaecologist in two weeks regarding operation procedures. Reading your story encouraged me a great deal.
Hi Helen, I hope you are well.
I finally had my surgery on August 14, 2023 after undergoing degeneration of fibroids which had me hospitalized for a week. The surgery was successful but the pain that came after was so intense, I felt like coughing but when I tried to do so, it hurt so much. I had to put a pillow on my tummy in order to somehow reduce the pain. I dare say the first week following the surgery is the toughest. Remembering this gave me some hope.
I had a foley to pass out my urine since I was not able to get up to walk after surgery. The third day after the surgery, I was able to get up and so the foley was removed. Walking was hard and painful but it became better as the days passed. I also experienced burning sensation while peeing for a couple of days like some other people shared. That was not pleasant at all.
I was privileged to have my mum with me while at the hospital and at home. She really helped with my recovery process. I’m wishing every woman a successful surgery and recovery process. You are not alone. Thank you Helen for having this platform.
Hello Helen! I was so glad to find your post; I have found so little on what to expect after a myomectomy! I had mine a week ago and my experience has been very similar… down to the bedsores on my bum! I also had the surgery 23 days before my 40th birthday and I loved to see you able to somewhat celebrate. Thanks for sharing this and keep living your best life!
Hope you are recovering well Maru! x
Thank you Helen for sharing your story , I m very grateful to you and all the ladies who shared their stories as well
the experience you shared was a great help for me as a person who went through the same experience with no clue , I went through a fibroid removal surgery last Monday so this is my 7th day after the surgery, I was in great pain the first 2 days , I hardly was able to get on my feet to go to the restroom but now I am much better .
I m 44 y old and I live in Egypt , it was very hard to find a similar content in Arabic where ladies can be open about sharing such personal experience and that’s why your words girls were my companion in the hospital .
My story started when I was making a routine ultrasound and I discovered a 5 cm fibroid in my uterus, the doctor said it is not a big deal and I can live with it especially if there is no bleedings or any side effects, one year later I found out that the fibroid became 9 cm but still no side effects , maybe I started to go to the make number one more frequently
My doctor said that it’s better to do the surgery cause it could grow bigger so I went for it , the first 3 days I was in great pain and may be even a little bit mad , because after the surgery I found out that the doctor made a vertical incision and not horizontal as he told me before and that made me made especially that his response was : ( oh , I didn’t tell you that !)
Call me shallow but I was really worried about the shape of my belly , in few days I convinced myself that health issues are the most important thing and I should be great full that it was not cancer and I was able to keep my uterus.
Now I am completing my recovery at home and I am still having a lot of worries in my mind especially that I still have a soft swollen part in my belly and I hope it’s not hernia ,
So for all the ladies who have fibroids and thinking about the surgery as an option … please :
– talk to more than one doctor before deciding if you are going under the knife especially open mastectomy and try to look at the pros and cons of the surgery especially if there is no side effect or pain or bleedings .
– if you decided to go through the surgery , collect info and write down all your questions in a piece of paper and ask them to your doctor , make him / her understand it’s your body , your decision.
– the first 2 days are the hardest , you will need a lot of painkillers beside antibiotics , you could feel abdominal muscles cramps beside the pain of the cut itself.
– it will take time for your system to reset and work again
My bladder started working on the 2nd day and I was unable to do number 2 till the 4th day .
– don’t ever ever get constipation.
– eating is not an easy process during the first 3 days .
– ask for help if yo need it .
– go easy and take very good care of yourself, spoil yourself if you can .
Hi everybody. Wow, this has been so helpful. I’m day 7 post op for 16cm and 8 cm fibroids and I have so many questions about what is normal in the healing process. Peeing is super unsatisfying…kind of dribbles out and never feels like I’ve emptied my bladder fully. Sort of like a UTI, but no burning sensation. A couple of you mentioned something like this, but not sure how it resolved? My bladder was heavily compromised, sharing space with fibroids, so I can imagine there is an adjustment period! Also, I have the strangest swelling around the incision that tends to concentrate, or settle on and below the incision when I’m standing or sitting but spreads out when I’m lying down. It’s almost like a shelf and feels like those stiff, but malleable stress balls.
I stopped the Tylenol and ibuprofen today and now have no desire to go for a walk. The pulling sensation is just too uncomfortable. I’m trying to stay positive, but the healing feels very, very slow. Thank you Helen and everybody for being so candid and generous with your stories! (I’m 52, btw)
Hi Helen, hope you’re doing great:)
Just read your story, Thank you so much love this has been so helpful. I also had a surgery 4 weeks ago, healing well. I have few questions regarding how and when to get or start my normal routine activity such as
● Intercourse(sex) when we resume
● Lying down on my stomach
● weight lifting limits because my lil one is 2½yr old only
● Bending down myself is safe?
● continues standing
May be you already mentioned those things and I missed out.. kindly reply me . I’ll be very grateful for your help ❤️
Thanks
Dear Helen,
I am 32 years old, and found out this year I have a 10.4 cm fibroid on the right side of my uterus. As of lately, I’ve been having urinary problems.
I am scheduled to see a urologist next month and then a gynecologist in November. I am unable to afford good insurance to get this sort of thing situated straight away! I am feeling a lot of uneasiness with all of this pain.
I struggle with my diet. I have been indulging lately in sugar and processed things like cheese, fried tortilla chips, ice cream, dark chocolate and canned sardines and canned beans. I keep cottage cheese on me at all times, it’s something I can’t get rid of because of the protein benefits I believe I get from it. My job is physical as well. I work at an airport outside in the sun, and I lift and stack/carry luggage, ranging from 10-50 pounds, and I’m on my knees a lot and such.
I have been slacking on my water intake lately as well!
Helen, I am hoping to have a great experience removing this, and getting relief from this fibroid I have. The ER doctor told me I have interstitial cystitis, but it could also be my fibroid causing these problems, as it is pushing down into my bladder.
My husband wants kids in the future, and I always say that I’m not sure…especially now that I have this!
Helen, I am so thankful to have come across this. I have saved it in my bookmarks to use as a reminder to be calm, and that a good moment will come for me, and to be thankful to God.
Much love.
Jos, 32 F from Santa Barbara, CA
Hi,
Thanks for your testimony as the same happened to my girlfriend this year (17cm myomectomy by laparotomy), and it helped me to better understand what we will face to after the surgery.
I have a question for you and all women experiencing this, did the myoma show up while you were having an IUD like Mirena ?
That was the case for my girlfriend, and I strongly suspect it : the pedunculated subserosal myoma was growing from the location where one of the branch of the IUD was touching/hurting the uterus (seen in MRI), her IUD was ectopic and displaced from the fundus to near the cervix.
Thanks and courage to all women experiencing this !
Ps : for those who read french I wrote an article on what happened to my girlfriend on my blog http://stormer.free.fr
Hello Helen! Love ur post just did mine last two weeks. Thanks for sharing. Love you
Helen, thank you so much for putting in the time to share your journey; especially the photos of your incision. I was just told that mine may not be a ridiculously large fibroid, but possibly enlarged uterus, ovary and there is a chance it may be cancerous. Because of the new possibilities and size of what they think are two (one 26 cm in diameter, the other 8 cm as of a month ago), though there is a possibility it is one with a branch that just looks like a separate entity they have now decided to make the incision similar to yours and oddly seeing how yours was healing make me feel hopeful that soon enough it’ll be not blatantly noticeable. Again, thank you for your bravery. You’ve helped more women than you’ll ever know ❤️